To get rid of acid reflux fast, you can take immediate actions like standing upright, loosening tight clothing, or using an over-the-counter antacid to neutralize stomach acid.
While occasional heartburn is common, persistent acid reflux can be a sign of a larger issue.
In fact, a nationwide study from Cedars-Sinai suggests that nearly a third of U.S. adults may experience it weekly.
This article provides a comprehensive guide to both immediate relief strategies and fast-acting lifestyle changes to manage and prevent the uncomfortable symptoms of acid reflux.
Continue reading to discover 10 detailed, evidence-based methods to take control of your acid reflux today.
In This Article
What Is Acid Reflux and What Causes It?
At its core, acid reflux is a mechanical failure. It occurs when the lower esophageal sphincter (LES), a muscular valve that acts as a gatekeeper between your esophagus and stomach, weakens or relaxes at the wrong time.
Normally, the LES opens to allow food to pass into the stomach and then promptly closes to prevent stomach contents from flowing backward.
When it malfunctions, potent stomach acid can flow back—or “reflux”—into the esophagus.
Because the esophageal lining is not designed to withstand this acidity, it becomes irritated, leading to the classic burning sensation known as heartburn.
It’s crucial to distinguish between occasional discomfort and a chronic condition. Occasional acid reflux, also known as gastroesophageal reflux (GER), is common and can happen to anyone, especially after a large or fatty meal.
However, when this reflux becomes frequent and disruptive, it is classified as gastroesophageal reflux disease (GERD).
The clinical definition for GERD is experiencing acid reflux symptoms more than twice a week.
Left unmanaged, GERD can lead to more severe complications, including inflammation of the esophagus (esophagitis), narrowing of the esophagus (strictures), and even an increased risk of esophageal cancer.
Several factors can contribute to the weakening of the LES and increase the risk of acid reflux.
According to research from institutions like the Mayo Clinic and academic reviews, key causes include:
- Hiatal Hernia: A condition where the upper part of the stomach bulges through an opening in the diaphragm, impairing the LES’s ability to close properly.
- Increased Abdominal Pressure: Conditions like obesity, pregnancy, and even wearing tight clothing can put physical pressure on the stomach, forcing its contents upward.
- Delayed Stomach Emptying: When food sits in the stomach for too long, it increases the likelihood of reflux.
- Lifestyle Factors: Smoking, consuming large meals, and eating certain trigger foods can all relax the LES or increase stomach acid production.
1. How Does Standing Up Straight Provide Instant Relief?
One of the simplest, fastest, and most effective ways to combat a sudden bout of acid reflux is to leverage the power of gravity.
When you are standing or sitting upright, gravity acts as a natural ally, helping to keep your stomach contents—including acid—down where they belong.
Slouching on the couch or, worse, lying down, effectively neutralizes this gravitational advantage, creating a level pathway for acid to travel from your stomach into your esophagus.
The Mechanism: Aiding Esophageal Clearance
The principle at play is known as esophageal clearance.
This is the body’s natural process of clearing any refluxed material back into the stomach through swallowing and peristalsis (the muscular contractions of the esophagus).
As documented in gastroenterology research, proper posture significantly aids this process.
When you stand up, you are not only preventing more acid from coming up but also helping your body clear what has already refluxed more efficiently.
How to Do It for Fast Relief
- Stop Slouching: The moment you feel the initial twinge of heartburn, make a conscious effort to correct your posture. If you’re sitting, sit up straight, pulling your shoulders back. If possible, stand up.
- Take a Gentle Walk: A slow, light walk for five to ten minutes can be even more beneficial. The gentle movement encourages digestion and allows gravity to work its magic on clearing the esophagus.
“Many patients report that the simple act of standing up and walking for 5-10 minutes after a meal significantly reduces the intensity of their heartburn, especially if they feel it coming on while seated.”
2. Why Does Loosening Your Clothing Help Acid Reflux?
This tip addresses a direct mechanical cause of acid reflux: excessive intra-abdominal pressure.
Tight clothing, particularly items that constrict the waistline like tight pants, high-waisted jeans, or snug belts, physically squeezes your abdomen.
This external pressure is transferred to your stomach, which can be enough to overcome a weakened LES and force stomach acid upward into the esophagus.
Think of your stomach as a flexible container. Squeezing it from the outside increases the internal pressure, making it more likely for its contents to escape through the top opening.
This is a simple but frequently overlooked factor that can trigger or worsen acid reflux symptoms, especially after a meal when the stomach is already full.
What to Do
- Immediate Action: As soon as you feel symptoms, provide immediate relief by unbuttoning your pants, loosening your belt by a notch or two, or changing into more comfortable, loose-fitting clothing like sweatpants or a dress.
- Preventative Tip: Be mindful of your wardrobe choices, especially on days you anticipate eating a larger meal. Opt for clothing with a comfortable, elastic waistband or avoid overly restrictive styles that put pressure on your midsection.
3. How Do Antacids Provide Fast Acid Reflux Relief?
For fast-acting chemical relief, over-the-counter (OTC) antacids are a go-to solution. Products like Tums®, Rolaids®, or Gaviscon® work by chemically neutralizing the acid already present in your stomach.
They contain alkaline compounds, such as calcium carbonate, magnesium hydroxide, or aluminum hydroxide, which are bases that counteract the acidity of your stomach’s hydrochloric acid.
This intervention is one of the quickest medical remedies available, often providing noticeable relief from heartburn within minutes.
It’s important to understand that antacids do not prevent the act of reflux itself, rather, they make the refluxed liquid less acidic and therefore less irritating and painful when it comes into contact with the esophageal lining.
According to sources like Healthline, they are ideal for managing occasional, infrequent heartburn.
Limitations and Considerations
While effective for rapid relief, antacids have limitations.
Their effect is temporary, typically lasting for only an hour or so.
They do not address the underlying mechanical issue with the LES, nor do they help heal any existing inflammation or damage to the esophagus.
Overuse of certain antacids can lead to side effects like constipation (from calcium or aluminum) or diarrhea (from magnesium).
They are a tool for acute symptom management, not a long-term solution for chronic GERD.
4. Can a Baking Soda Solution Act as a Quick Remedy?
A common home remedy that operates on the same principle as OTC antacids is a simple baking soda solution.
Baking soda, or sodium bicarbonate, is a natural base.
When mixed with water and ingested, it reacts with stomach acid (hydrochloric acid) to neutralize it, producing salt, water, and carbon dioxide.
This can provide very fast, albeit temporary, relief from the burning sensation of heartburn.
How-To Guide
- Mix 1/2 teaspoon of baking soda into a 4-ounce (120 ml) glass of cold water.
- Stir vigorously until the powder is completely dissolved.
- Sip the solution slowly. Drinking it too quickly can introduce a large amount of gas into the stomach, potentially causing bloating and belching.
Crucial Disclaimer: This remedy should be used with extreme caution and only for occasional, acute symptoms. Due to its very high sodium content, it is not safe for individuals on a low-sodium diet, or those with high blood pressure, kidney disease, or heart failure. Overuse can disrupt the body’s delicate acid-base balance and lead to metabolic alkalosis. It is not a substitute for medical advice or a long-term management strategy.
5. How Does Chewing Gum Help Fight Acid Reflux?
This may seem like an old wives’ tale, but there is solid science behind the recommendation to chew gum after a meal to combat acid reflux.
The benefit is twofold and centers on stimulating the production of saliva.
The Dual-Benefit Mechanism
- Neutralization: Saliva is naturally slightly alkaline because it contains bicarbonate. As you chew gum, your salivary glands go into overdrive. The increased flow of alkaline saliva travels down your esophagus, helping to neutralize any acid that has refluxed from the stomach.
- Clearance: The act of chewing gum also makes you swallow more frequently. Each swallow helps to physically wash or “clear” the acid back down into the stomach, speeding up the esophageal clearance process we discussed earlier.
Multiple studies have validated this simple strategy.
For it to be effective, it’s important to choose sugar-free gum to avoid contributing to dental cavities.
Chewing a piece for about 30 minutes after a meal can significantly reduce post-meal acid exposure in the esophagus.
6. Why Is Elevating Your Head the Key to Stopping Nighttime Reflux?
Nighttime acid reflux can be particularly troublesome, disrupting sleep and causing more severe symptoms like coughing, choking, or a sore throat in the morning.
The primary culprit is lying flat. In this position, your esophagus and stomach are at the same horizontal level, creating an easy, gravity-free path for stomach acid to flow backward.
The solution is to elevate not just your head, but your entire upper torso.
This creates an incline that forces stomach acid to fight gravity to reach your esophagus, a battle it is much less likely to win.
As confirmed by numerous studies and clinical guidelines from sources like the National Center for Biotechnology Information (NCBI), this is one of the most effective lifestyle modifications for managing GERD.
The Right Way vs. The Wrong Way
- The Wrong Way: Simply stacking a few regular pillows. This typically only bends your neck forward, which can actually increase pressure on your abdomen and potentially make reflux worse. It does not create the necessary straight incline for your torso.
- The Right Way: The goal is a gradual, stable incline from the waist up. This can be achieved in two effective ways:
- Use a Wedge Pillow: These are triangular foam pillows specifically designed to elevate the upper body by 6 to 8 inches. They provide a consistent and comfortable slope.
- Elevate the Bed Frame: Place sturdy blocks of wood or bed risers securely under the legs at the head of your bed frame to raise the entire head of the bed by 6-8 inches.

7. Why Must You Avoid Lying Down After Eating?
The timing of your meals relative to when you lie down is a critical factor in managing acid reflux.
After you eat, your stomach is full and actively producing a significant amount of acid to begin the digestive process.
If you lie down within 2 to 3 hours of a meal, you create a perfect storm for acid reflux symptoms: a full stomach combined with a lack of gravitational assistance.
Furthermore, large meals can cause the stomach to stretch, a phenomenon known as gastric distension.
This stretching can decrease the resting pressure of the LES, making it less effective at staying tightly closed.
When you add a horizontal posture to this scenario, the risk of significant reflux increases dramatically.
This is why late-night dinners or snacks are a common trigger for many people.
Practical Advice
Make it a rule to finish your last meal of the day, or any large snack, at least 3 hours before you go to bed or lie down on the couch.
This gives your stomach ample time to digest and empty a significant portion of its contents, reducing both the volume and the pressure that could lead to reflux.
8. How Do Smaller Meals Prevent Acid Reflux Flare-Ups?
The size of your meals has a direct impact on the function of your lower esophageal sphincter (LES).
Eating a large meal stretches the stomach, which can trigger a physiological event known as transient lower esophageal sphincter relaxations (TLESRs).
As detailed in advanced gastroenterology literature from StatPearls and other NCBI sources, TLESRs are brief, involuntary openings of the sphincter that are not related to swallowing.
They are a primary mechanism behind reflux in both healthy individuals and those with GERD, and their frequency increases significantly after large, fatty meals.
By eating smaller, more frequent meals, you avoid over-distending the stomach.
This reduces the primary trigger for TLESRs and keeps the pressure within the stomach at a more manageable level, placing less strain on the LES.
This proactive strategy is less about immediate relief and more about preventing flare-ups from happening in the first place.
Actionable Strategy
Instead of the traditional three large meals per day, try shifting to five or six smaller “mini-meals” spaced throughout the day.
This approach helps maintain stable energy levels, prevents extreme hunger, and, most importantly, keeps your stomach from becoming overly full, thereby reducing the mechanical and physiological triggers for acid reflux.
9. How Do You Identify and Avoid Your Trigger Foods?
While there is a list of common culprits, food triggers for acid reflux are highly individual.
What causes severe heartburn in one person may be perfectly fine for another.
Therefore, one of the most powerful and personalized strategies for long-term management is to become a detective of your own diet and identify your specific triggers.
Across numerous health sources, including Yale Medicine and the Mayo Clinic, a consensus list of common triggers has emerged.
These foods tend to either relax the LES, increase stomach acid production, or delay stomach emptying.
Common Triggers to Watch For:
- High-Fat or Fried Foods: These slow down digestion, leaving food in the stomach longer. (e.g., fast food, bacon, cheese)
- Spicy Foods: Can irritate the esophageal lining directly. (e.g., chili, hot sauces)
- Tomatoes and Tomato-Based Products: Highly acidic. (e.g., marinara sauce, ketchup, salsa)
- Citrus Fruits: Also highly acidic. (e.g., oranges, lemons, grapefruit, pineapple)
- Chocolate & Peppermint: Both are known to relax the LES muscle.
- Coffee & Caffeinated Tea: Can increase stomach acid and relax the LES.
- Carbonated Beverages & Alcohol: Carbonation can increase stomach pressure, and alcohol can relax the LES.
How to Identify Your Personal Triggers
- Keep a Food and Symptom Diary: For at least one week, meticulously log everything you eat and drink, the time you consume it, and any acid reflux symptoms you experience, noting their severity and timing.
- Look for Patterns: At the end of the week, review your diary. Do your symptoms consistently appear after you eat spicy food? Does your morning coffee seem to be the culprit?
- Eliminate and Test: Once you identify a suspected trigger, completely eliminate it from your diet for a full week. If your symptoms improve, you’ve likely found a culprit. You can later try reintroducing it in a small amount to confirm its effect.
10. Can Breathing Exercises Really Help Acid Reflux?
This is a more advanced and novel strategy, but one that is gaining support in the medical community.
The connection lies in the relationship between your diaphragm—the large muscle at the base of your lungs that controls breathing—and your LES.
The diaphragm actually wraps around the LES, providing crucial external support to the sphincter. This is part of the body’s natural anti-reflux barrier.
If diaphragmatic function is weak or uncoordinated, this external support can falter, contributing to a higher likelihood of reflux.
Research, including a systematic review cited by the Mayo Clinic, suggests that deep, diaphragmatic breathing exercises can strengthen this muscle.
A stronger diaphragm can, in turn, help reinforce the barrier function of the LES, reducing the frequency of reflux episodes.
A Simple Diaphragmatic Breathing Exercise
- Lie comfortably on your back with your knees bent and feet flat on the floor.
- Place one hand on your upper chest and the other on your belly, just below your rib cage.
- Inhale slowly and deeply through your nose. Focus on allowing your belly to rise as it fills with air, while keeping the hand on your chest as still as possible. This ensures you are using your diaphragm.
- Exhale slowly through pursed lips (as if you were whistling), feeling your belly gently fall.
- Repeat this process for 5 to 10 minutes daily. Consistency is key to strengthening the muscle over time.
Comparative Table: Foods to Avoid vs. Foods That Soothe Acid Reflux
Navigating diet can be confusing. This table provides a clear comparison of common trigger foods and those that are generally considered soothing and less likely to cause acid reflux symptoms.
| Foods That Often Trigger Acid Reflux Symptoms | Foods That May Help Soothe and Prevent Symptoms |
|---|---|
| Fatty & Fried Foods (e.g., fast food, bacon) | High-Fiber Foods (e.g., oatmeal, brown rice, sweet potatoes) |
| Spicy Foods (e.g., chili, hot sauces, curry) | Alkaline Foods (e.g., bananas, melons, cauliflower, nuts) |
| Citrus Fruits (e.g., oranges, lemons, grapefruit) | Watery Foods (e.g., cucumber, lettuce, celery, watermelon) |
| Tomato-Based Products (e.g., marinara, ketchup) | Ginger (in moderation, as tea or grated into food) |
| Chocolate & Peppermint | Lean Proteins (e.g., grilled chicken, fish, tofu) |
| Coffee & Caffeinated Tea | Healthy Fats (e.g., avocado, walnuts, olive oil) |
| Carbonated Beverages & Alcohol | Non-Citrus Fruits (e.g., apples, pears, berries in moderation) |
| Onions & Garlic (especially raw) | Herbal Teas (e.g., chamomile, licorice root) |
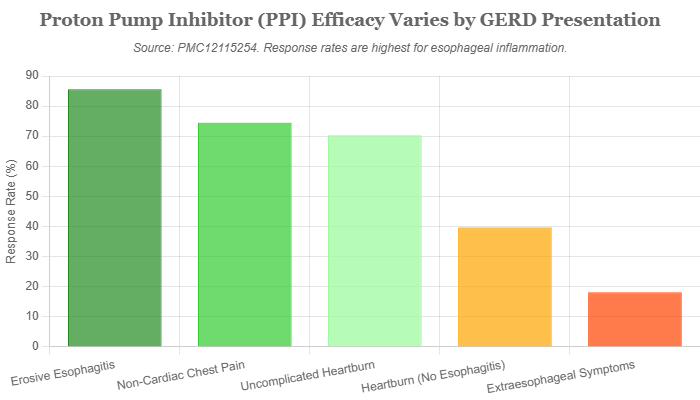
The chart above illustrates a critical point in managing GERD: the effectiveness of standard medications like Proton Pump Inhibitors (PPIs) can vary dramatically. While highly effective for healing physical inflammation in the esophagus (erosive esophagitis), their success rate drops for symptoms without visible damage or for those outside the esophagus, highlighting why lifestyle interventions are so crucial.
When Should You See a Doctor for Acid Reflux?
While the tips in this article can provide fast and effective relief for occasional acid reflux, it is absolutely crucial to seek professional medical advice if your symptoms are frequent, severe, or persistent.
Self-treating a chronic condition can be dangerous, as it may mask a more serious underlying problem or allow complications to develop unchecked.
Consult a healthcare professional if you experience any of the following:
- You experience heartburn or other acid reflux symptoms more than twice per week. This is the clinical threshold for GERD.
- Over-the-counter medications are not providing adequate relief, or you find yourself needing to take them on a daily basis.
- Your symptoms interfere with your daily life or disrupt your sleep.
- You experience any “alarm symptoms” which can indicate serious complications and require immediate medical evaluation. These symptoms, highlighted by major health organizations, include:
- Difficulty swallowing (dysphagia)
- Painful swallowing (odynophagia)
- Unexplained weight loss
- A persistent sensation of a lump or food being stuck in your throat (globus sensation)
- Vomiting, especially if it contains blood or material that looks like coffee grounds
- Stools that are black, tarry, or contain visible blood
- Anemia (low iron levels)
- A chronic cough, persistent hoarseness, or new or worsening asthma that doesn’t respond to typical treatments.
Frequently Asked Questions (FAQ)
What causes acid reflux at night?
Lying flat removes the helpful effect of gravity, allowing stomach acid to flow more easily into the esophagus. The body also naturally produces less saliva and you swallow less frequently during sleep, which reduces the natural mechanisms that clear acid away from the esophagus.
Can drinking water help with acid reflux?
Yes, in moderation. Drinking a small amount of water can help dilute stomach acid and wash it back down from the esophagus. However, drinking a large volume of water can fill the stomach and increase internal pressure, potentially worsening reflux symptoms.
Is it acid reflux or a heart attack?
While heartburn causes a burning chest pain, a heart attack often feels like intense pressure, squeezing, or fullness. Heart attack pain may radiate to the jaw, neck, or arms and is often accompanied by shortness of breath, cold sweats or lightheadedness. If you have any doubt, seek emergency medical help immediately.
What is the difference between acid reflux and GERD?
Acid reflux is the event of stomach acid flowing backward into the esophagus. GERD (Gastroesophageal Reflux Disease) is the chronic, more severe form of this condition, typically diagnosed when reflux symptoms occur more than twice a week or when they lead to complications like inflammation.
Can stress and anxiety make acid reflux worse?
Yes. While stress doesn’t directly cause the mechanical failure of the LES, it can increase stomach acid production and heighten your perception of pain, making heartburn feel more severe. Managing stress through techniques like meditation or the breathing exercises mentioned above can be very beneficial.
Why do I still have symptoms even on PPI medication?
This is a common issue. A Cedars-Sinai study found over half of patients on daily PPIs still had symptoms. Reasons can include not taking the medication correctly (it’s most effective 30-60 minutes before a meal), the presence of non-acid reflux (reflux of bile), or having a different condition that mimics GERD.
What are the “alarm symptoms” I should never ignore?
Never ignore difficulty swallowing, painful swallowing, unexplained weight loss, signs of bleeding (like vomiting blood or black stools), or a persistent feeling of food being stuck. These require immediate medical attention to rule out serious complications like strictures or cancer.
Are there any natural remedies that are scientifically supported?
Yes. Lifestyle modifications like weight management, elevating the head of the bed, and avoiding trigger foods are strongly supported by evidence. Chewing sugar-free gum and trying ginger in moderation are also backed by some studies. Many other popular remedies, however, lack robust scientific proof.
Conclusion
In summary, you can get rid of acid reflux fast by using a multi-pronged approach that addresses the immediate symptoms and underlying triggers.
The most effective strategies involve a combination of immediate actions like standing up and loosening clothing, fast-acting solutions like OTC antacids for acute episodes, and smart preventative habits like modifying your diet, meal timing and sleeping posture.
By understanding the mechanical and physiological reasons behind your symptoms, you can make targeted changes that yield significant results.
Start by implementing one or two of these evidence-based strategies today to feel immediate relief.
Remember, while these tips are powerful tools for management, they are not a cure.
If your symptoms persist, are severe, or you experience any alarm symptoms, it is essential to consult a healthcare professional to get an accurate diagnosis and a comprehensive, personalized treatment plan.
What’s the one tip you’re going to try first? Share your experience in the comments below!
Reference
[1] Gastroesophageal reflux disease (GERD) – Symptoms and causes
https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940
[2] Gastroesophageal Reflux Disease (GERD) – StatPearls
https://www.ncbi.nlm.nih.gov/books/NBK554462
[3] Definition & Facts for GER & GERD – NIDDK
[4] Gastroesophageal Reflux Disease (GERD) – PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC6140167
[5] LPT: If you have heartburn or acid reflux, swallow some air … – Reddit
[6] GERD (Gastroesophageal Reflux Disease) – Yale Medicine
https://www.yalemedicine.org/conditions/gerd-gastroesophageal-reflux-disease
[7] Heartburn and Indigestion (Dyspepsia) – Self Care Forum
https://www.selfcareforum.org/heartburn-and-indigestion/
[8] Acid Reflux & GERD Treatment Online | Amwell for Patients

