A brain aneurysm is a weak, bulging spot on the wall of an artery in the brain.
While the thought of having one can be frightening, it’s important to know that many people live with unruptured aneurysms without any issues.
In fact, according to the Cleveland Clinic, up to 6% of people in the U.S. have an unruptured brain aneurysm.
The real danger arises when an aneurysm leaks or bursts, causing a life-threatening type of stroke.
Understanding this condition is the first step toward managing risk and recognizing warning signs.
This comprehensive guide will walk you through everything you need to know about a brain aneurysm.
We will explore what it is, the different types, the critical differences in symptoms between a stable and a ruptured aneurysm, and the risk factors that contribute to their formation and rupture.
You will also learn about modern diagnostic techniques, advanced treatment options, and what the latest scientific research tells us about the future of aneurysm care.
Continue reading to empower yourself with knowledge that could be life-saving.
In This Article
What Exactly Is a Brain Aneurysm?
A brain aneurysm, also known as a cerebral aneurysm or intracranial aneurysm, is a bulge or “ballooning” that forms in a weak area of a blood vessel wall within the brain.
The constant pressure of blood flowing through the artery pushes this weakened section outward, creating a blister-like sac filled with blood.
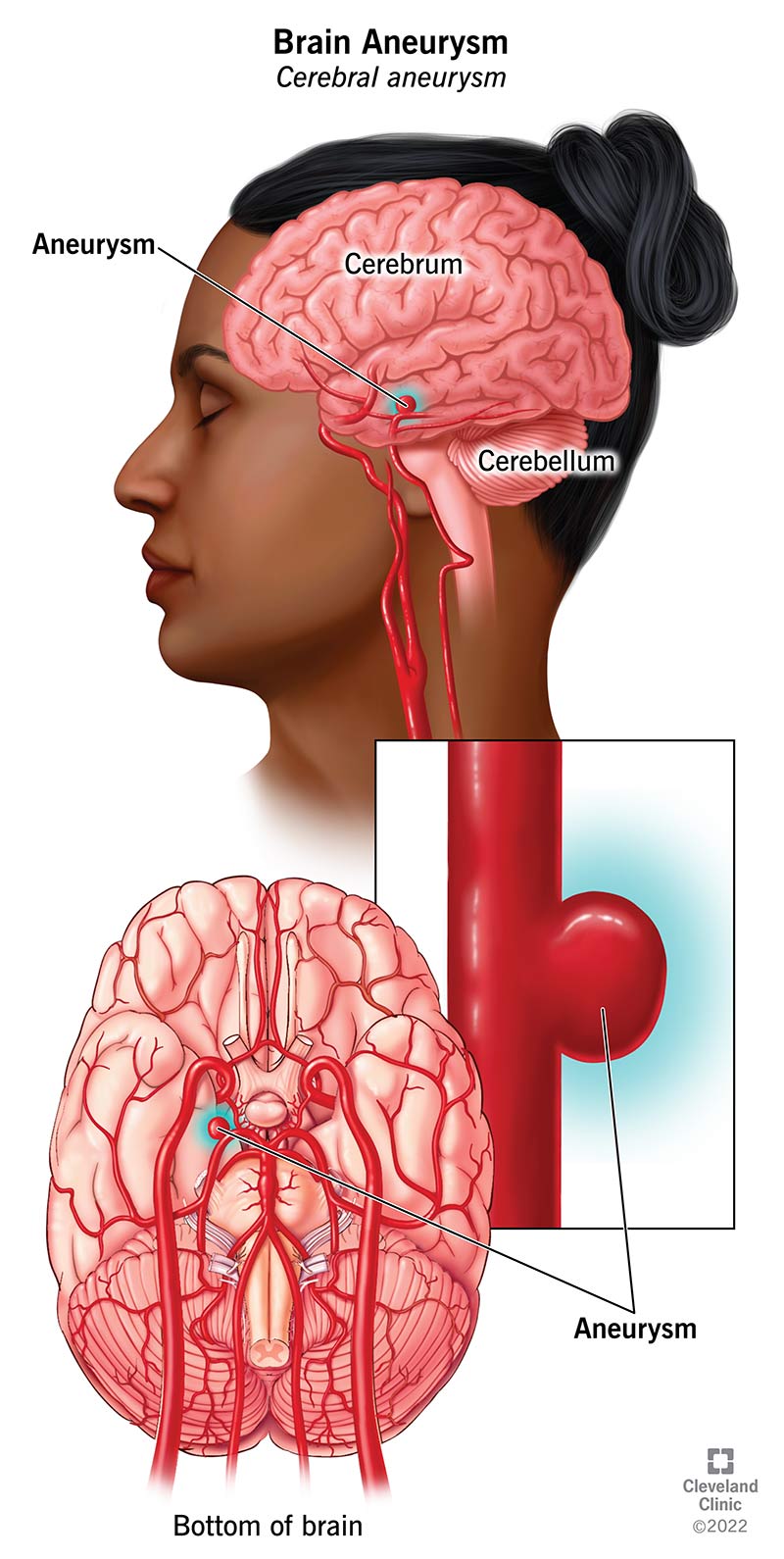
A brain aneurysm is a bulge in a weak area of an artery.
The “Balloon in the Brain” Analogy
A helpful way to visualize a brain aneurysm is to think of a balloon.
As you fill a balloon with air, its walls stretch and become thinner. If one spot on the balloon is weaker than the rest, it will bulge out more and be at a higher risk of popping.
Similarly, as blood rushes into a brain aneurysm, it stretches the thin, weakened arterial wall, increasing the risk that it could leak or rupture.
How and Where Do They Form?
Brain aneurysms often form at the forks or branches of arteries, as these points are naturally weaker and subject to more hemodynamic stress.
While they can occur anywhere in the brain, most are found in the major arteries along the base of the skull.
According to information from the National Institute of Neurological Disorders and Stroke (NINDS), this location is where the brain’s primary blood supply network, the Circle of Willis, is situated.
Unruptured vs. Ruptured Aneurysms
It’s crucial to distinguish between an unruptured and a ruptured brain aneurysm, as their implications are vastly different.
- Unruptured Aneurysm: This is an aneurysm that remains intact. The majority of brain aneurysms are unruptured and small (less than 11 millimeters). They often produce no symptoms and are frequently discovered by chance during imaging tests for other medical conditions. While they have the potential to rupture, many never do.
- Ruptured Aneurysm: This is a medical emergency. When an aneurysm ruptures, it releases blood into the space surrounding the brain, an event called a subarachnoid hemorrhage (SAH). This bleeding increases pressure inside the skull, can damage brain cells directly, and can lead to severe complications like stroke, coma, and death.
Ruptured Aneurysm: A Medical Emergency
A ruptured brain aneurysm is life-threatening. The primary symptom is a sudden, extremely severe headache, often described as “the worst headache of my life”. If you or someone you know experiences this, especially with other symptoms like nausea, stiff neck, or loss of consciousness, call 911 or your local emergency number immediately.
What Are the Different Types of Brain Aneurysms?
Healthcare professionals classify brain aneurysms based on their shape and, in some cases, their cause.
They are also categorized by size, which is a key factor in assessing rupture risk.
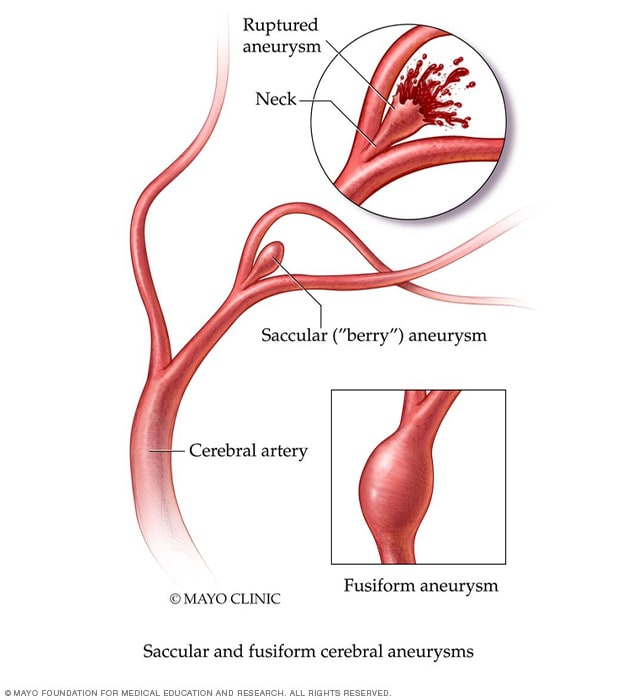
The most common types of brain aneurysms are saccular and fusiform.
Types by Shape
The three main types of brain aneurysms based on their form are:
- Saccular Aneurysm: Also known as a “berry aneurysm”, this is the most common type. It looks like a round, blood-filled sac or “berry” hanging from a narrow neck or stem, protruding from a main artery or one of its branches. Saccular aneurysms typically form on arteries at the base of the brain.
- Fusiform Aneurysm: This type involves a ballooning or bulging of the artery on all sides, without a distinct “neck”. It appears as a spindle-shaped widening of the entire vessel segment. These are less common than saccular aneurysms.
- Mycotic Aneurysm: This is a rare type of aneurysm caused by an infection in the arterial wall. The infection, which can spread from elsewhere in the body, weakens the artery, causing it to bulge.
Classification by Size
The size of a brain aneurysm is a critical factor in determining its risk of rupture and the best course of treatment.
According to NINDS, they are generally classified as:
- Small: Less than 11 millimeters in diameter (about the size of a large pencil eraser).
- Large: 11 to 25 millimeters in diameter (about the width of a dime).
- Giant: Greater than 25 millimeters in diameter (larger than the width of a quarter).
While larger aneurysms have a higher risk of rupture, it’s important to note that even small aneurysms can burst.
The growth of an aneurysm, regardless of its initial size, is considered a significant risk factor.
What Are the Symptoms of a Brain Aneurysm?
The symptoms of a brain aneurysm depend entirely on whether it is unruptured, leaking, or has fully ruptured.
Many people with an unruptured brain aneurysm have no symptoms at all.
Symptoms of an Unruptured Brain Aneurysm
Most small, stable unruptured aneurysms are asymptomatic.
However, if an aneurysm grows large enough, it can press on adjacent brain tissue or nerves, causing neurological symptoms. These may include:
- Pain above and behind one eye
- A dilated (enlarged) pupil in one eye
- Blurred or double vision
- Numbness, weakness, or paralysis on one side of the face
- A drooping eyelid
- Chronic headaches
If you experience any of these symptoms, it is important to see a healthcare provider for evaluation.
Symptoms of a “Leaking” Aneurysm (Sentinel Bleed)
In some cases, an aneurysm may leak a small amount of blood into the brain.
This is known as a sentinel bleed and can produce a sudden, severe headache called a “sentinel headache”.
This headache can serve as a warning sign that a major rupture may be imminent, often occurring days or weeks beforehand.
However, only a minority of patients experience a sentinel headache before a full rupture.
Symptoms of a Ruptured Brain Aneurysm
A ruptured brain aneurysm causes a sudden and catastrophic set of symptoms due to bleeding in the brain.
This is a medical emergency requiring immediate attention.
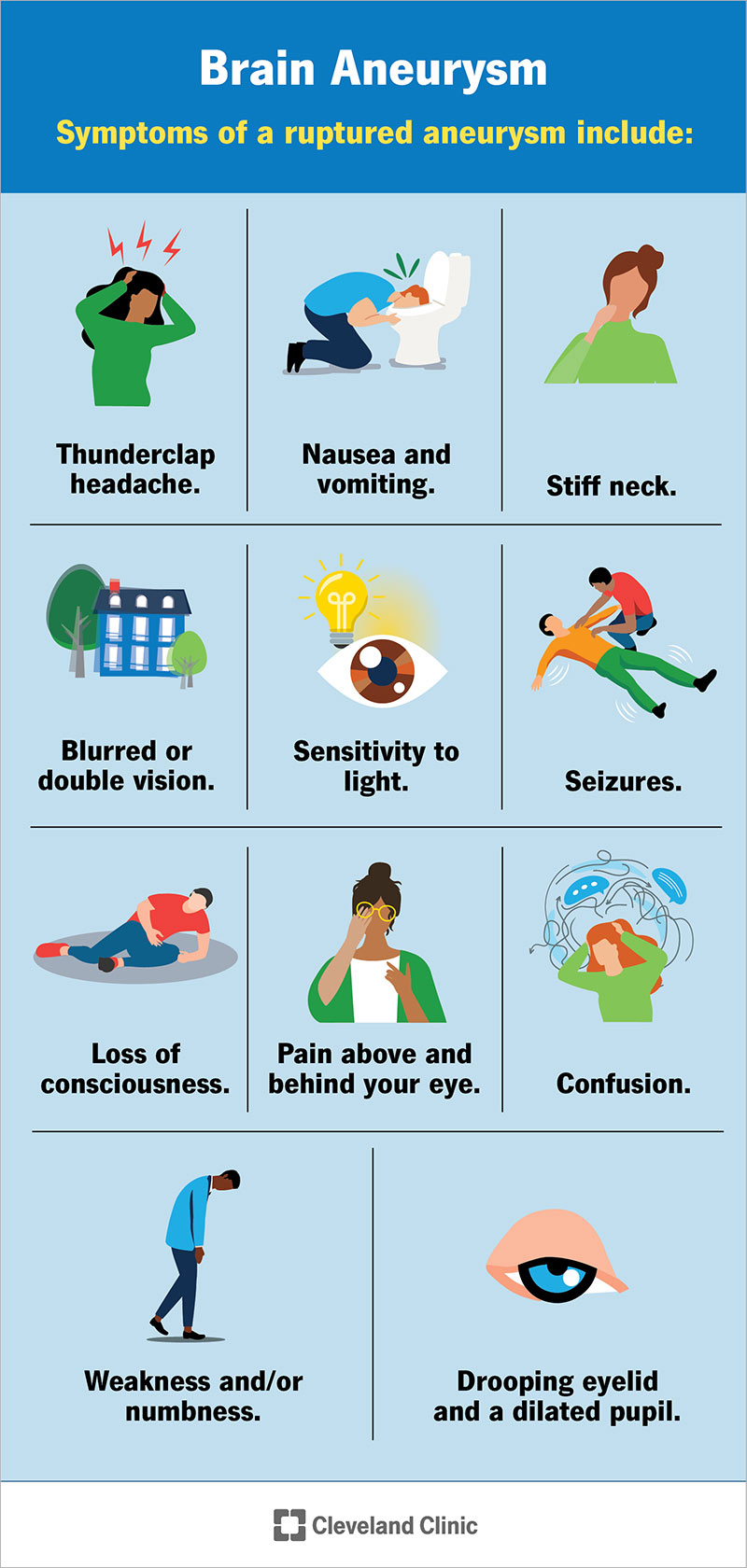
Symptoms of a ruptured aneurysm are sudden and severe.
The hallmark symptom is a sudden, excruciating headache, which many people describe as “the worst headache of my life”. This is often referred to as a thunderclap headache.
Other symptoms that can accompany the headache include:
- Nausea and vomiting
- Stiff neck
- Blurred or double vision
- Extreme sensitivity to light (photophobia)
- Seizures
- A drooping eyelid
- Confusion or disorientation
- Loss of consciousness (brief or prolonged)
- Cardiac arrest (in severe cases)
What Causes a Brain Aneurysm and Who Is at Risk?
A brain aneurysm forms when an artery wall thins and weakens.
This weakness can be present at birth or develop over a lifetime due to a combination of genetic predispositions and lifestyle factors.
Risk Factors for Developing an Aneurysm
A risk factor is anything that increases your chance of developing a medical condition.
Having one or more risk factors does not guarantee you will develop a brain aneurysm, but it does increase the likelihood. Key risk factors include:
- Cigarette Smoking: Smoking is one of the strongest modifiable risk factors. It damages blood vessel walls and is linked to both the formation and rupture of aneurysms.
- High Blood Pressure (Hypertension): Uncontrolled high blood pressure exerts constant force on artery walls, which can cause weak spots to form and bulge over time.
- Family History: Having a first-degree relative (parent, sibling, or child) with a brain aneurysm increases your risk. The risk is even higher if two or more first-degree relatives are affected.
- Age: Aneurysms are most commonly diagnosed in adults between the ages of 30 and 60.
- Gender: Brain aneurysms are more common in women than in men, particularly after menopause, suggesting a possible hormonal link.
- Inherited Connective Tissue Disorders: Conditions like Ehlers-Danlos syndrome and Marfan syndrome weaken the body’s connective tissues, including those in blood vessel walls.
- Polycystic Kidney Disease (PKD): This inherited disorder, which causes cysts to form in the kidneys, is also associated with an increased risk of brain aneurysms.
- Drug Use: The use of stimulant drugs, especially cocaine and amphetamines, can dramatically raise blood pressure and cause inflammation in the arteries, contributing to aneurysm formation.
- Excessive Alcohol Consumption: Heavy alcohol use can also contribute to high blood pressure.
What Causes a Brain Aneurysm to Rupture?
Not all aneurysms will rupture. The decision to treat an unruptured aneurysm often involves weighing the risk of rupture against the risks of the treatment itself.
Several factors are known to increase the likelihood of a rupture:
| Risk Factor | Description |
|---|---|
| Aneurysm Size and Shape | Large, giant, and irregularly shaped aneurysms (e.g., those with smaller “daughter sacs” budding off) are more likely to rupture than small, smooth, round ones. |
| Aneurysm Growth | An aneurysm that is observed to be growing over time on follow-up imaging is considered to be at a higher risk of rupture, regardless of its initial size. This is a major indicator for treatment. |
| Location | Aneurysms located on certain arteries, such as the posterior communicating artery and the anterior communicating artery, have a higher statistical risk of rupture. |
| Previous Rupture | If a person has already experienced a ruptured aneurysm or a sentinel bleed, the risk of a re-bleed or rupture of another existing aneurysm is significantly higher. |
| High Blood Pressure | Untreated or poorly controlled hypertension is a leading cause of rupture. Sudden spikes in blood pressure from straining or intense emotion can be a trigger. |
| Smoking | Continuing to smoke significantly increases the risk that an existing aneurysm will rupture. |
How Is a Brain Aneurysm Diagnosed?
The diagnostic process for a brain aneurysm depends on the situation.
For a patient presenting with symptoms of a rupture, the goal is rapid confirmation of bleeding. For asymptomatic patients, aneurysms are often found incidentally.
If a rupture is suspected, a doctor will immediately order tests to check for blood in the space around the brain. The primary diagnostic tools include:
- Computed Tomography (CT) Scan: This is usually the first and fastest test performed in an emergency setting. A non-contrast CT scan can quickly reveal if there has been bleeding into the brain (a subarachnoid hemorrhage).
- CT Angiography (CTA): If the initial CT shows bleeding, a CTA is often performed. This involves injecting a contrast dye into a vein and taking detailed CT images of the brain’s arteries. The CTA can show the precise location, size, and shape of the aneurysm that has ruptured.
- Cerebrospinal Fluid (CSF) Analysis: If a CT scan is negative but a rupture is still strongly suspected, a doctor may perform a lumbar puncture (spinal tap). A sample of the cerebrospinal fluid that surrounds the brain and spinal cord is drawn and analyzed for the presence of red blood cells, which would confirm bleeding.
- Cerebral Angiography (Digital Subtraction Angiography – DSA): This is the gold standard for visualizing brain aneurysms. A catheter is inserted into an artery (usually in the groin or wrist) and guided up to the arteries in the brain. Contrast dye is injected directly, providing highly detailed, real-time X-ray images of the blood vessels. This test gives the most accurate information about the aneurysm’s anatomy, which is critical for planning treatment.
- Magnetic Resonance Imaging (MRI) / Magnetic Resonance Angiography (MRA): MRI and MRA use a strong magnetic field and radio waves to create detailed images. While not typically the first test in an emergency, MRA is an excellent non-invasive tool for detecting and monitoring unruptured aneurysms.
How Is a Brain Aneurysm Treated?
Treatment for a brain aneurysm is highly individualized.
The decision depends on whether the aneurysm has ruptured, its size, location, and shape, as well as the patient’s age and overall health.
Treating a Ruptured Brain Aneurysm
A ruptured aneurysm is a medical emergency that requires immediate treatment to secure the aneurysm and prevent re-bleeding, which is often fatal.
The primary goal is to stop blood from flowing into the aneurysm sac. The two main approaches are:
1. Surgical (Microvascular) Clipping
This is an open-brain surgery performed by a neurosurgeon.
The surgeon removes a small section of the skull (a craniotomy) to access the aneurysm.
Using a powerful microscope, the surgeon identifies the blood vessel feeding the aneurysm and places a tiny, clothespin-like metal clip across the neck of the aneurysm.
This clip permanently seals it off from the artery, preventing blood from entering. Once an aneurysm is completely clipped, it typically does not come back.
2. Endovascular Coiling
This is a less invasive procedure performed from inside the blood vessels by a neurosurgeon or interventional neuroradiologist.
A catheter is inserted into an artery in the groin or wrist and navigated to the aneurysm in the brain.
Through this catheter, the specialist carefully deploys tiny, soft platinum wires (coils) into the aneurysm sac.
The coils fill the aneurysm, promoting blood clotting and sealing it off from the inside.
Sometimes, a stent (a mesh tube) or a balloon is used to help hold the coils in place.
Aneurysms treated with coiling can sometimes recur, requiring further treatment.
Other Advanced Endovascular Treatments
- Flow Diversion: For large or complex aneurysms, a special stent called a flow diverter can be placed in the parent artery across the aneurysm’s neck. This fine-mesh stent diverts blood flow away from the aneurysm, causing it to gradually shrink and clot off over time.
- WEB Device: The Woven EndoBridge (WEB) device is a newer technology. It is a small, mesh-like cube or sphere that is placed inside a wide-necked aneurysm. It works similarly to coils by disrupting blood flow and promoting clotting to seal the aneurysm.
Treating an Unruptured Brain Aneurysm
Not all unruptured aneurysms require immediate treatment.
For small aneurysms with a low estimated risk of rupture, a doctor may recommend a “watch and wait” approach. This involves:
- Regular Monitoring: Using non-invasive imaging like MRA or CTA at regular intervals (e.g., annually) to check for any growth or changes in the aneurysm’s shape.
- Aggressive Risk Factor Management: This is the most critical part of conservative management. It includes strict blood pressure control, immediate smoking cessation, and managing cholesterol and other medical conditions.
If an unruptured aneurysm is large, growing, causing symptoms, or if the patient has significant risk factors (like a family history of rupture), preventative treatment with clipping, coiling, or flow diversion may be recommended.
The decision is made after a thorough discussion of the risks and benefits of treatment versus observation.
What Is the Outlook for Someone with a Brain Aneurysm?
The prognosis, or outlook, for a person with a brain aneurysm varies dramatically depending on whether it ruptures.
Prognosis for an Unruptured Aneurysm
For individuals with a small, unruptured brain aneurysm that is not treated, the prognosis is generally excellent.
Many people live their entire lives without the aneurysm ever causing a problem.
The key is diligent monitoring and strict management of risk factors like high blood pressure and smoking.
Prognosis for a Ruptured Aneurysm
The outlook after a rupture is far more serious.
A ruptured brain aneurysm is a devastating event with high rates of mortality and disability. According to the Cleveland Clinic, the statistics are sobering:
- Approximately 25% of people die within 24 hours of a rupture.
- Up to 50% of people die within three months, often due to complications.
- Of those who survive, about 66% are left with some form of permanent neurological deficit or brain damage.
Factors that influence the outcome include the patient’s age and health before the rupture, the severity of the initial bleed, how quickly treatment is received, and the development of complications like vasospasm (narrowing of brain arteries after the bleed) and hydrocephalus (buildup of fluid in the brain).
Can You Prevent a Brain Aneurysm?
While you cannot change genetic risk factors like family history or inherited disorders, you can take significant steps to lower your risk of developing a brain aneurysm or causing an existing one to rupture.
Prevention focuses on maintaining the health of your blood vessels.
Key preventative measures include:
- Do Not Smoke: If you smoke, quitting is the single most important thing you can do. If you don’t smoke, don’t start.
- Control Your Blood Pressure: Work with your healthcare provider to maintain a healthy blood pressure through diet, exercise, and medication if necessary.
- Avoid Stimulant Drug Use: Do not use cocaine, amphetamines, or other illicit drugs that cause dangerous spikes in blood pressure.
- Limit Alcohol Intake: Moderate your alcohol consumption, as excessive use can raise blood pressure.
- Eat a Heart-Healthy Diet: A diet low in saturated fat and high in fruits, vegetables, and whole grains helps maintain vascular health.
If you have a strong family history of brain aneurysms, speak with your doctor about the possibility of screening with a non-invasive test like an MRA.
What Is the Latest Research on Brain Aneurysms?
The field of neurovascular medicine is constantly evolving.
Research funded by organizations like the National Institute of Neurological Disorders and Stroke (NINDS) is focused on better understanding, diagnosing, and treating brain aneurysms.
Current areas of intense research include:
- Genetics and Genomics: Scientists are working to identify specific genes and genetic variations that predispose individuals to aneurysm formation. This could lead to better screening for at-risk families.
- Predictive Modeling: Researchers are developing sophisticated computational models that use imaging data (like size and shape) and blood flow dynamics to more accurately predict which specific aneurysms are likely to grow and rupture. This will help personalize treatment decisions.
- Advanced Imaging and Biomarkers: The goal is to develop non-invasive imaging techniques or blood tests (biomarkers) that can identify inflammation or instability in an aneurysm wall, signaling a high risk of rupture before it happens.
- Improving Treatments: Ongoing studies are aimed at making current treatments safer and more effective. This includes developing better coils, more flexible flow diverters, and new medications that can promote healing or prevent complications like vasospasm.
- Hormonal Influences: Given the higher prevalence in postmenopausal women, researchers are investigating how hormones like estrogen may have a protective effect on blood vessels and how this knowledge could be used therapeutically.
Frequently Asked Questions (FAQ)
1. Can a brain aneurysm go away on its own?
It is extremely rare for a brain aneurysm to shrink or disappear on its own. Most either remain stable or grow larger over time. This is why monitoring is essential if one is not treated.
2. Can stress cause a brain aneurysm to rupture?
While chronic stress isn’t a direct cause of formation, a sudden surge in blood pressure from intense stress or anger can be a trigger for the rupture of a pre-existing aneurysm.
3. What is the survival rate of a ruptured brain aneurysm?
The survival rate is approximately 50%. Of those who survive, a significant portion experience long-term neurological disabilities. Rapid medical treatment is critical to improving the odds of survival and recovery.
4. Can you feel a brain aneurysm in your head?
Most unruptured aneurysms cause no sensation. Only if an aneurysm becomes very large and presses on nerves might it cause localized pain (like behind the eye), but you cannot “feel” the aneurysm itself.
5. Is it safe to fly with an unruptured brain aneurysm?
For most people with a small, stable, unruptured aneurysm, flying is considered safe. The pressure changes in a commercial aircraft cabin are not significant enough to pose a risk. However, you should always discuss this with your neurologist.
6. How long is recovery after brain aneurysm surgery?
Recovery varies widely. For an unruptured aneurysm treated with coiling, it may be a few days to weeks. After open surgery (clipping) for an unruptured aneurysm, it’s typically two to four weeks. Recovery from a ruptured aneurysm is much longer, often taking many months to a year or more and involving extensive rehabilitation.
7. Can you live a normal life after brain aneurysm treatment?
Many people who undergo successful preventative treatment for an unruptured aneurysm return to a completely normal life. After a rupture, the ability to live a “normal” life depends on the extent of the initial brain injury and the success of rehabilitation.
8. Are headaches a sign of a brain aneurysm?
Chronic daily headaches are not a typical symptom of an unruptured aneurysm. The key warning sign is a sudden, severe “thunderclap” headache, which signals a rupture and requires immediate emergency care.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for, and should never be relied upon for, professional medical advice. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.

