When facing hearing loss, the path to better hearing can seem complex. Two of the most discussed solutions are hearing aids and cochlear implants.
While both aim to improve hearing, they operate on fundamentally different principles.
A hearing aid amplifies sound to assist a damaged ear, whereas a cochlear implant bypasses the damaged parts of the inner ear to directly stimulate the auditory nerve.
This distinction is critical. With approximately 15% of American adults reporting some trouble hearing, understanding the right solution is more important than ever.
For many, hearing aids are a life-changing, non-invasive first step. But for those with severe to profound hearing loss, a cochlear implant may offer a sense of sound that even the most powerful hearing aids cannot provide.
This article will provide a comprehensive, evidence-based comparison of these two technologies.
We will delve into how they work, who they are for, the associated costs and procedures, expected outcomes, and the risks involved, empowering you to have a more informed conversation with your healthcare provider.
In This Article
What Is a Hearing Aid and How Does It Work?
A hearing aid is a small electronic device that you wear in or behind your ear.
It is designed for individuals with mild to severe hearing loss, but whose inner ear (cochlea) and auditory nerve are still functional enough to process sound when it’s made louder and clearer.
The Basic Principle: Amplification
The core function of a hearing aid is amplification. It uses a microphone to pick up sounds from the environment, an amplifier to increase the volume of those sounds, and a receiver (a tiny speaker) to deliver the amplified sound into the ear canal.
Modern digital hearing aids are highly sophisticated, capable of selectively amplifying certain frequencies where hearing loss is greatest, reducing background noise, and adapting to different listening environments.
“Hearing aids amplify sounds so they may be detected by damaged ears. They do not bypass any part of the hearing system but rather make sounds loud enough for the remaining healthy hair cells in the cochlea to detect.” – Based on information from the National Institute on Deafness and Other Communication Disorders (NIDCD).
Key Components of a Hearing Aid
Most hearing aids, regardless of style, share three main parts:
- Microphone: Captures sound waves from the air and converts them into electrical signals.
- Amplifier: Increases the strength of the electrical signals. A digital processor within the amplifier customizes the sound based on the user’s specific hearing loss profile.
- Receiver (Speaker): Converts the amplified electrical signals back into sound waves and delivers them into the ear.
Types of Hearing Aids
Hearing aids come in various styles, and the choice often depends on the degree of hearing loss, lifestyle, cosmetic preferences, and dexterity.
According to a 2025 analysis by Forbes Health, common types include:
- Behind-the-Ear (BTE): The most common type. A plastic case sits behind the ear, connected by a tube to a custom earmold or a dome that fits in the ear canal. Suitable for almost all types of hearing loss.
- Receiver-in-Canal (RIC): Similar to a BTE, but the receiver is placed directly in the ear canal, connected by a thin wire. This often results in a more natural sound quality.
- In-the-Ear (ITE): Fills most of the bowl-shaped area of the outer ear. Its larger size can accommodate more features and is easier to handle.
- In-the-Canal (ITC): A smaller, custom-molded device that fits partly in the ear canal.
- Completely-in-Canal (CIC): Molded to fit inside the ear canal, making it one of the most discreet options.
In recent years, the market has also opened up to Over-the-Counter (OTC) hearing aids, which are intended for adults with perceived mild to moderate hearing loss and do not require a prescription.
Who Is a Good Candidate for a Hearing Aid?
A person is generally a good candidate for hearing aids if they:
- Have mild, moderate, or severe sensorineural hearing loss.
- Still have a functioning auditory nerve and enough healthy inner ear hair cells to process amplified sound.
- Experience difficulty understanding speech, especially in noisy environments.
- Find that turning up the volume on the TV or radio helps them hear better.
The primary goal of a hearing aid is to make speech and environmental sounds audible and clear, thereby improving communication and overall quality of life.
What Is a Cochlear Implant and How Does It Work?
A cochlear implant is a complex, surgically implanted medical device designed for individuals with severe to profound sensorineural hearing loss who receive little to no benefit from conventional hearing aids.
It is not a hearing aid, it does not amplify sound. Instead, it provides a sense of sound by bypassing the damaged parts of the inner ear and directly stimulating the auditory nerve.
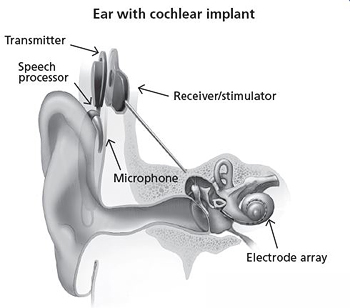
A cochlear implant consists of an external processor and a surgically placed internal implant.
The Basic Principle: Bypassing Damage
In severe to profound hearing loss, the delicate hair cells inside the cochlea (the snail-shaped organ of the inner ear) are often extensively damaged or absent.
These cells are responsible for converting sound vibrations into electrical signals for the brain.
Since no amount of amplification can make these damaged cells work, hearing aids become ineffective. A cochlear implant circumvents this problem entirely.
“Cochlear implants bypass damaged portions of the ear and directly stimulate the auditory nerve. Signals generated by the implant are sent by way of the auditory nerve to the brain, which recognizes the signals as sound.” – National Institute on Deafness and Other Communication Disorders (NIDCD)
Key Components of a Cochlear Implant
A cochlear implant system has two main parts, as detailed by both the NIDCD and the Mayo Clinic:
1. The External Component
This part is worn behind the ear or off-the-ear on the scalp. It consists of:
- A Microphone: Picks up sound from the environment.
- A Speech Processor: Selects, analyzes, and digitizes the sounds picked up by the microphone.
- A Transmitter: Held in place by a magnet, it sends the processed sound signals wirelessly through the skin to the internal device.
2. The Internal (Implanted) Component
This part is placed under the skin via a surgical procedure. It includes:
- A Receiver/Stimulator: Receives the signals from the external transmitter and converts them into electrical impulses.
- An Electrode Array: A thin wire with a group of electrodes that is carefully threaded into the cochlea. These electrodes deliver the electrical impulses to different regions of the auditory nerve.
The Sound’s Journey: From Microphone to Brain
- Sound is captured by the external microphone.
- The speech processor converts the sound into a special digital code.
- The transmitter sends this code across the skin to the internal receiver.
- The receiver converts the code into electrical impulses.
- The electrode array sends these impulses to different parts of the auditory nerve.
- The auditory nerve carries the signals to the brain, which interprets them as sound.
It’s important to note that hearing through a cochlear implant is different from normal hearing and takes time and intensive therapy to learn or relearn.
Users often initially describe the sound as “robotic” or “artificial”, but the brain adapts over time.
Who Is a Good Candidate for a Cochlear Implant?
Candidacy for a cochlear implant is determined through a thorough evaluation. Generally, candidates include children and adults who:
- Have severe to profound sensorineural hearing loss in one (unilateral) or both (bilateral) ears.
- Receive little or no benefit from appropriately fitted hearing aids. This is often measured by poor speech recognition scores (e.g., understanding less than 50-60% of words in a sentence test).
- Are motivated and have realistic expectations about the outcomes.
- Are healthy enough to undergo surgery and participate in post-implant rehabilitation.
The FDA has approved cochlear implants for children as young as 9 months old, as early implantation can be critical for developing speech and language skills during a key developmental window.
What Are the Key Differences at a Glance?
Understanding the core distinctions between hearing aids and cochlear implants is the first step in navigating your hearing health options.
This table provides a clear, side-by-side comparison of the most important factors.
| Feature | Hearing Aids | Cochlear Implants |
|---|---|---|
| Primary Function | Acoustically amplify sound. | Electrically stimulate the auditory nerve. |
| Mechanism | Makes sounds louder for the existing hearing system to process. | Bypasses the damaged inner ear to send signals directly to the brain. |
| Target Hearing Loss | Mild to severe sensorineural hearing loss. | Severe to profound sensorineural hearing loss. |
| Procedure | Non-surgical. Fitted by an audiologist. | Surgical procedure required to place the internal components. |
| Sound Perception | Makes natural sound louder and clearer. | Provides a representation of sound that the brain learns to interpret. Initially may sound “robotic”. |
| Candidacy | Functional inner ear hair cells and auditory nerve are required. | Used when hair cells are too damaged for hearing aids to be effective. A functional auditory nerve is essential. |
| Average Cost (2025) | $1,000 – $8,000 per pair (prescription), $300 – $2,000 (OTC). | $40,000 – $100,000+ per ear (including device, surgery, and therapy). |
| Insurance Coverage | Often not covered by basic Medicare or many private plans. | Typically covered by Medicare and most private insurance plans as a prosthetic device. |
| Rehabilitation | Adjustment period and follow-up appointments. | Extensive, mandatory post-operative therapy with audiologists and speech-language pathologists. |
How Do You Qualify for a Cochlear Implant vs. a Hearing Aid?
The journey to either a hearing aid or a cochlear implant begins with a comprehensive evaluation.
However, the criteria and the process for each are vastly different, reflecting the distinct nature of the interventions.
The Evaluation Process for Hearing Aids
Qualifying for a hearing aid is a relatively straightforward process, typically involving:
- Audiogram: A hearing test conducted by an audiologist to map your hearing thresholds across different frequencies. This determines the type and severity of your hearing loss.
- Speech Testing: Tests to assess how well you understand words and sentences in both quiet and noisy environments.
- Lifestyle Assessment: A discussion with your audiologist about your communication needs, work environment, social activities, and budget to help select the most appropriate technology.
If the results show a hearing loss that can be helped by amplification and there are no medical contraindications, the audiologist will recommend and fit appropriate hearing aids.
The Rigorous Candidacy Evaluation for a Cochlear Implant
Determining candidacy for a cochlear implant is a much more in-depth, multidisciplinary process.
As outlined by the Mayo Clinic, the evaluation team typically includes an ENT surgeon and an audiologist, and the process involves:
- Audiological Evaluation: This includes an audiogram and, crucially, speech recognition tests performed while wearing appropriately fitted, powerful hearing aids. A key indicator for a cochlear implant referral is poor performance on these tests.
- The 60/60 Guideline: Many audiologists use a simple screening tool known as the 60/60 guideline. As explained by HearingUp, this suggests a referral for a cochlear implant evaluation if a patient has hearing loss of 60 decibels (dB) or greater and a word recognition score of 60% or less in their better-hearing ear.
- Medical Examination: An ENT surgeon examines the ear to ensure there are no active infections or other issues that would complicate surgery. The surgeon also discusses the risks and benefits of the procedure.
- Imaging Scans (CT or MRI): These scans of the head and inner ear are performed to check the anatomy of the cochlea and ensure the electrode array can be safely inserted.
- Psychological and Social Evaluation: This assesses the candidate’s (or their family’s) motivation, expectations, and support system, which are all critical for successful rehabilitation.
When Hearing Aids Aren’t Enough: The Tipping Point
Key Takeaway
The critical factor for cochlear implant candidacy is not just the severity of hearing loss on an audiogram, but poor speech understanding despite using powerful hearing aids. If you can hear sounds but cannot make sense of words, it’s a strong sign that amplification alone is insufficient and a cochlear implant evaluation may be warranted.
A study published in Otology & Neurotology found that after implantation, the average word perception ability improved from 8.2% pre-surgery to 53.9% post-surgery, demonstrating the profound impact a cochlear implant can have when hearing aids are no longer effective.
What Does the Cochlear Implant Surgery and Recovery Involve?
Unlike hearing aids, receiving a cochlear implant involves a surgical procedure and a structured recovery and rehabilitation process.
While the surgery is now considered routine and safe, it’s a significant step that requires careful preparation and commitment.
Preparing for Surgery
Before the procedure, your surgical team will provide detailed instructions. According to the Mayo Clinic, preparation typically includes:
- Reviewing medications and supplements, and stopping certain ones like blood thinners.
- Fasting (no food or drink) for a set period before surgery.
- Arranging for transportation home, as you cannot drive after receiving general anesthesia.
- Receiving recommended vaccinations, such as for meningitis, to reduce the risk of rare but serious post-operative infections.
The Surgical Procedure Step-by-Step
The surgery is performed by an otolaryngologist (ENT surgeon) under general anesthesia and typically takes about two to three hours per ear.
- Incision: The surgeon makes a small incision behind the ear.
- Mastoidectomy: A small hole is drilled in the mastoid bone behind the ear to create a path to the middle ear.
- Cochleostomy: A tiny opening is made into the cochlea, the snail-shaped structure of the inner ear.
- Electrode Insertion: The surgeon carefully threads the electrode array of the cochlear implant into the cochlea.
- Receiver Placement: The internal receiver/stimulator is secured under the skin behind the ear.
- Closure: The incision is closed with stitches.
Most patients can go home the same day or after a one-night stay in the hospital.
Post-Surgery: The Healing Period
The initial recovery period lasts for a few weeks. During this time, you might experience some pressure, discomfort, or numbness around the implant site, as well as temporary dizziness or nausea.
The external sound processor is not worn during this healing phase. The focus is on allowing the incision to heal completely before the device is activated.
“Activation Day”: Turning on the Device
This is a milestone moment that occurs about 2 to 4 weeks after surgery. An audiologist will:
- Fit the external speech processor.
- Turn on the cochlear implant for the first time.
- Create a “map” for the processor, which involves setting the stimulation levels for each electrode so that sounds are audible but comfortable.
- Provide instructions on how to care for and use the device.
The first sounds heard can be strange and overwhelming. As one patient’s father described in a Mayo Clinic video, “Hi, beautiful. Can you hear me? It’s Daddy”.
The initial response is just the beginning of a long journey of the brain learning to interpret these new signals.
The Crucial Role of Rehabilitation and Therapy
Receiving a cochlear implant is not a simple “switch-on” solution.
The brain needs to be trained to understand the new electrical signals it’s receiving. This process, known as aural rehabilitation, is essential for success.
“This involves training your brain to understand the sounds you hear through the cochlear implant. At first speech and everyday noises around you won’t sound the same as you might recall them… This process is ongoing.” – Mayo Clinic
Rehabilitation involves regular sessions with audiologists and speech-language pathologists. For adults who lost hearing later in life, it’s a process of re-learning.
For young children, it’s a process of learning speech and language for the first time. Success is highly dependent on this therapeutic commitment.
What Are the Costs and Insurance Coverage for Each Device?
The financial investment for hearing aids and cochlear implants differs dramatically, as does the way they are typically handled by insurance providers.
This is one of the most significant practical differences between the two technologies.
The Cost of Hearing Aids in 2025
The price of hearing aids can vary widely based on technology level, features, and service model (bundled vs. unbundled).
Based on 2025 data from sources like Forbes and HearingTracker, here’s a general breakdown:
- Over-the-Counter (OTC) Hearing Aids: Ranging from $300 to $2,000 per pair, these are for adults with self-perceived mild to moderate hearing loss.
- Prescription Hearing Aids: The average cost is typically between $2,000 and $8,000 per pair. This price often includes professional services like the hearing test, fitting, and follow-up adjustments.
Insurance for Hearing Aids: Coverage is inconsistent. Traditional Medicare (Part A and B) does not cover hearing aids.
Some Medicare Advantage (Part C) plans offer partial benefits, and coverage varies widely among private insurance plans. Many people pay for hearing aids out-of-pocket.
The Cost of a Cochlear Implant: A Comprehensive Breakdown
The cost of a cochlear implant is substantially higher because it includes the device, a surgical procedure, and extensive post-operative care.
According to CareCredit, the total cost in the United States can range from $40,000 to over $100,000 per ear.
This comprehensive cost typically covers:
- Pre-surgical evaluations and consultations.
- The internal implant and external processor.
- Surgeon’s fees and hospital/facility charges.
- Anesthesia.
- Post-operative activation and initial programming (“mapping”).
- Aural rehabilitation and speech therapy sessions.
Insurance for Cochlear Implants: This is a key differentiator. Because a cochlear implant is a surgically implanted prosthetic device used to treat a medical condition (profound deafness), it is typically covered by insurance. As the American Cochlear Implant Alliance notes:
- Medicare provides coverage for cochlear implants for qualifying candidates.
- Over 90% of private insurance plans cover cochlear implantation.
- Medicaid, TRICARE, and the VA also provide coverage.
While coverage is generally robust, patients will still be responsible for deductibles, copayments, and coinsurance, which can vary significantly by plan.
What Are the Outcomes and Benefits of Each Device?
Both hearing aids and cochlear implants can dramatically improve quality of life, but the specific benefits and expected outcomes align with the type of hearing loss they are designed to treat.
Hearing Aid Benefits: Improving Audibility and Quality of Life
For individuals with mild to severe hearing loss, hearing aids offer significant benefits:
- Improved Communication: Making speech easier to understand in most situations.
- Enhanced Safety: Better awareness of environmental sounds like alarms, traffic, and sirens.
- Reduced Listening Effort: Less mental fatigue from straining to hear.
- Cognitive Health: A landmark 2023 study published in The Lancet (the ACHIEVE study) showed that for older adults at increased risk for cognitive decline, using hearing aids slowed cognitive decline by 48% over three years. A separate meta-analysis in JAMA Neurology found that using hearing restorative devices was associated with a 19% decrease in the risk of long-term cognitive decline.
Cochlear Implant Benefits: Restoring a Sense of Sound and Speech Clarity
For those with severe to profound hearing loss, a cochlear implant can be transformative, offering benefits beyond the reach of hearing aids:
- Improved Speech Understanding: This is the primary goal. A study cited by Cochlear Americas found that at 12 months post-implantation, 97% of adults experienced significant improvement in speech understanding compared to their pre-implant performance with hearing aids.
- Hearing Environmental Sounds: The ability to hear footsteps, the doorbell, birds singing, and other sounds that contribute to a sense of connection and safety.
- Ability to Use the Telephone: Many users regain the ability to have conversations over the phone.
- Enjoyment of Music: While challenging, many modern cochlear implant users learn to enjoy and even create music.
- Improved Tinnitus: Many patients report a reduction in the ringing or buzzing in their ears (tinnitus) when using the device.
Patient Satisfaction and Real-World Experiences
The ultimate measure of success is how these devices impact daily life.
A global survey reported by The Hearing Review found that 96% of cochlear implant users expressed overall satisfaction with their devices. The journey requires patience, but the results can be profound.
“For me, it’s what brings me to work every day… To people in that room, witnessing Aida hear for the first time was to witness a miracle.” – Melissa DeJong, Au.D., commenting on a child’s cochlear implant activation at the Mayo Clinic.
A scoping review of 201 studies concluded that “it is evident that cochlear implantation is beneficial to the majority of adults of any age who have limited aided speech perception abilities”.
What Are the Risks and Limitations to Consider?
While both technologies offer immense benefits, it is crucial to have a balanced understanding of their potential risks and limitations.
The decision to pursue either option should be made with full awareness of the potential downsides.
Risks and Limitations of Hearing Aids
Hearing aids are non-invasive and very safe, but they are not without limitations:
- Limited Effectiveness for Profound Loss: Their primary limitation is that they cannot help when the inner ear is too damaged to process sound, no matter how much it is amplified.
- Sound Quality Issues: Users may experience feedback (whistling), occlusion (a feeling of being plugged up), or difficulty in very noisy situations.
- Maintenance: They require regular cleaning, battery changes or charging, and occasional repairs.
- Stigma: Although diminishing, some individuals still feel a social stigma associated with wearing hearing aids.
Risks and Limitations of a Cochlear Implant
As a surgical procedure, a cochlear implant carries more significant risks, which are thoroughly reviewed with every candidate.
The U.S. Food and Drug Administration (FDA) and the Mayo Clinic list potential risks including:
Surgical Risks (Rare)
- Infection: Infection at the incision site or, very rarely, meningitis (inflammation of the membranes surrounding the brain).
- Facial Nerve Damage: The facial nerve passes through the ear, and there is a small risk of temporary or permanent weakness or paralysis on the side of the surgery.
- Dizziness or Balance Problems: The inner ear’s balance system can be temporarily or sometimes permanently affected.
- Tinnitus: Ringing in the ear may develop or worsen.
- Cerebrospinal Fluid Leak: A rare complication where fluid from around the brain leaks.
Device and Hearing-Related Risks
- Loss of Residual Hearing: The implantation process often destroys any remaining natural hearing in the implanted ear. This is a critical consideration for candidates who still have some usable low-frequency hearing.
- Device Failure: Although reliable, the internal device can fail, requiring another surgery to replace it.
- Uncertain Long-Term Effects: The long-term effects of electrical stimulation on the auditory nerve are not fully known, though decades of use have shown it to be safe.
- Variable Outcomes: Not everyone achieves the same level of success. Performance can vary widely, and some may not benefit as much as others.
Living with a cochlear implant also requires a lifelong commitment to device maintenance, regular appointments with an audiologist for mapping adjustments, and protecting the external processor from water and impact.
What Does the Future Hold for Hearing Technology?
The field of hearing technology is evolving at a rapid pace. Both hearing aids and cochlear implants are benefiting from advances in microelectronics, battery technology, and artificial intelligence.
Advances in Hearing Aid Technology
The future of hearing aids is focused on personalization and seamless integration:
- Artificial Intelligence (AI): Hearing aids are becoming smarter, using AI to automatically adapt to the listener’s environment, distinguishing between speech and noise with greater accuracy.
- Enhanced Connectivity: Direct Bluetooth streaming from smartphones, TVs, and other devices is now standard, turning hearing aids into personalized audio headsets.
- Biometric Sensors: Future devices may incorporate sensors to track health metrics like physical activity, heart rate, and even detect falls.
- The OTC Market: The growth of the Over-the-Counter market is expected to drive innovation and accessibility for those with mild to moderate hearing loss.
The Next Generation of Cochlear Implants
Research for cochlear implants, supported by institutions like the NIDCD, is focused on improving sound quality and expanding candidacy:
- Totally Implantable Systems: Researchers are working on developing a cochlear implant where all components, including the microphone and processor, are under the skin, making the device completely invisible.
- Hearing Preservation: New, more delicate electrode arrays and surgical techniques are being developed to preserve any remaining low-frequency hearing a patient might have. This allows for a combination of acoustic (hearing aid) and electric (cochlear implant) stimulation in the same ear, known as “hybrid” or “electro-acoustic stimulation (EAS)”.
- Improved Music and Tonal Language Perception: Future processing strategies aim to provide a richer, more nuanced sound quality that better represents the complexities of music and tonal languages.
- Bimodal Hearing: Research continues to show the benefits of pairing a cochlear implant in one ear with a hearing aid in the other, which can improve hearing in noise and sound localization.
Conclusion
The choice between a hearing aid and a cochlear implant is not a matter of which is “better”, but which is appropriate for an individual’s specific type and degree of hearing loss. They are two different tools for two different jobs.
- Hearing aids are the standard of care for most people with hearing loss, working by amplifying sound for an ear that can still process it. They are non-invasive, highly advanced, and effective for mild to severe hearing loss.
- A cochlear implant is a life-changing medical intervention for those whom hearing aids are no longer enough. It is for individuals with severe to profound hearing loss, bypassing the damaged inner ear to provide a sense of sound directly to the brain.
The most important step you can take is to seek a professional evaluation from an audiologist.
They can accurately diagnose your hearing loss and guide you toward the right solution. If you are a hearing aid user who still struggles to understand conversations, don’t hesitate to ask about a cochlear implant evaluation.
Understanding all your options is the key to unlocking a world of better hearing and improved quality of life.
We encourage you to share this article with anyone who might benefit from this information and to leave your questions or experiences in the comments below.
Frequently Asked Questions (FAQ)
1. Can you wear a hearing aid and a cochlear implant at the same time?
Yes. This is called “bimodal hearing”, where a person wears a cochlear implant in one ear and a hearing aid in the other. This combination can improve sound localization and hearing in noisy environments by blending the electrical stimulation of the implant with the acoustic sound from the hearing aid.
2. Does a cochlear implant restore normal hearing?
No. A cochlear implant does not restore normal hearing. It provides a useful representation of sound that the brain learns to interpret. The sound quality is different from natural hearing, but it allows most users to understand speech and perceive environmental sounds effectively after rehabilitation.
3. How long does a cochlear implant last?
The internal, surgically implanted component is designed to last a lifetime. The external processor, like any electronic device, typically lasts five to ten years and can be upgraded as technology improves without needing another surgery. New processors are designed to be compatible with older internal implants.
4. Can adults who have been deaf since birth benefit from a cochlear implant?
Adults with prelingual deafness (deaf before learning to speak) generally have more variable outcomes than those who lost hearing later in life. While they may not achieve the same level of speech understanding, many still gain significant benefits, such as improved awareness of environmental sounds and enhanced lip-reading ability.
5. What is the youngest age a child can receive a cochlear implant?
In the United States, the FDA has approved cochlear implants for eligible children beginning at 9 months of age. Early implantation is crucial as it exposes the brain to sound during the critical period for speech and language development, leading to better long-term outcomes.
6. Is the cochlear implant surgery painful?
The surgery is performed under general anesthesia, so there is no pain during the procedure. Post-operative discomfort, pressure, or mild pain around the implant site is common but is typically well-managed with pain medication and subsides within a few days.
7. Will I be able to swim with a cochlear implant?
The internal implant is completely safe in water. The external processor is not waterproof and must be removed before swimming or showering. However, many manufacturers offer waterproof accessories, such as special cases or sleeves, that allow users to wear their processor while swimming.
8. How much do hearing aids cost?
The cost varies greatly. In 2025, Over-the-Counter (OTC) hearing aids range from about $300 to $2,000 per pair. Prescription hearing aids, which include professional services, typically cost between $2,000 and $8,000 per pair, depending on the technology level.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for, and should never be relied upon for, professional medical advice. Always talk to your doctor or a qualified audiologist about any questions you may have regarding a medical condition or treatment options.