A varicocele is an enlargement of the veins within the scrotum, the loose bag of skin that holds the testicles.
This condition is the most common correctable cause of male infertility, affecting approximately 15-20% of the general male population.
While often painless and harmless, a varicocele can sometimes lead to pain, testicular atrophy (shrinkage) and significant fertility issues.
Understanding this common condition is the first step toward effective management and preserving reproductive health.
This comprehensive guide will explore every facet of varicocele, from its subtle symptoms and underlying causes to the most advanced diagnostic techniques.
We will provide a detailed comparison of all available treatment options, including watchful waiting, minimally invasive embolization and state-of-the-art microsurgery.
By the end of this article, you will have a clear, authoritative understanding of varicocele and the steps you can take to address it.
In This Article
What Is a Varicocele? (A Deeper Definition)
A varicocele (VAR-ih-koe-seel) is essentially a varicose vein of the scrotum. It occurs when the veins within the spermatic cord, known as the pampiniform plexus, become enlarged and dilated.
The job of these veins is to transport oxygen-depleted blood away from the testicles.
When the one-way valves inside these veins fail or function poorly, blood can flow backward and pool, causing the veins to swell and create a varicocele.
This condition is far more common on the left side (around 80-90% of cases) due to the anatomical path the left testicular vein takes.
It typically develops during puberty and can grow larger and more noticeable over time.
While many men with a varicocele have no symptoms and experience no health issues, for others it can be a source of significant concern.
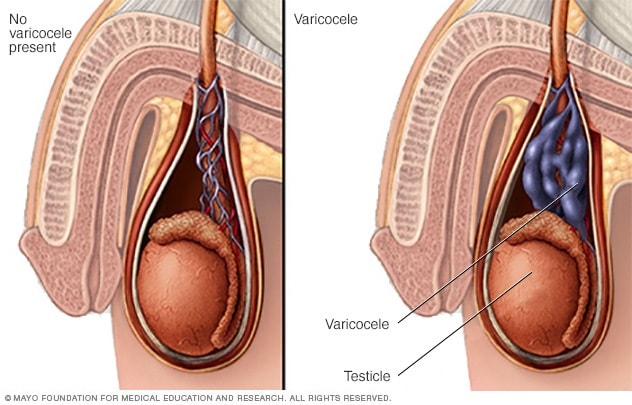
A varicocele is an enlargement of the veins that transport oxygen-depleted blood away from the testicle.
The “Bag of Worms”: What Does It Look and Feel Like?
The most classic description of a palpable varicocele is that it feels like a “bag of worms” within the scrotum.
This description, while unusual, is quite accurate for larger varicoceles.
The collection of swollen, twisted veins can create a soft, lumpy mass that is usually located above the testicle.
- Visual Appearance: For a large varicocele, the enlarged veins may be visible through the scrotal skin, especially when standing. The affected side of the scrotum might appear fuller or hang lower.
- Feel by Touch: When palpated, the texture is often described as a bundle of soft, squiggly tubes. It is typically not tender to the touch unless it is causing pain.
- Changes with Position: A varicocele is often more prominent when a person is standing up for a long time, due to gravity increasing the pressure in the veins. It may become less noticeable or disappear completely when lying down, as the blood can drain more easily.
It’s important to note that smaller varicoceles may not be visible or easily felt and are often discovered only during a medical examination or through an ultrasound.
How a Varicocele Forms: The Role of Veins and Valves
To understand how a varicocele forms, it’s helpful to understand the circulatory system of the testicles.
Arteries deliver oxygen-rich blood to the testicles, while a network of veins, the pampiniform plexus, carries the oxygen-depleted blood away.
This plexus also plays a crucial role in temperature regulation, acting as a heat exchanger to keep the testicles slightly cooler than the core body temperature, which is essential for healthy sperm production.
These veins contain tiny, one-way valves that are supposed to ensure blood flows in the right direction—up and away from the testicles toward the heart.
A varicocele develops when these valves fail. This condition is known as venous insufficiency.
When the valves don’t close properly, gravity causes blood to flow backward and pool in the pampiniform plexus.
This backflow, or reflux, increases the pressure within the veins, causing them to stretch, dilate, and twist, forming a varicocele.
Varicocele vs. Varicose Veins: Understanding the Similarity
A varicocele is fundamentally the same type of problem as varicose veins that commonly appear in the legs.
Both conditions are caused by venous insufficiency, where faulty valves lead to blood pooling and vein enlargement.
The primary difference is the location and the specific set of symptoms and complications they cause.
- Varicose Veins (Legs): Typically cause cosmetic concerns, aching, swelling and in severe cases, skin ulcers or blood clots.
- Varicocele (Scrotum): While sometimes causing pain, the main clinical significance of a varicocele is its potential to impair testicular function, leading to reduced sperm production and infertility.
What Are the Common Symptoms of a Varicocele?
Many varicoceles produce no signs or symptoms and are often discovered incidentally during a routine physical exam or an infertility evaluation.
However, when symptoms do occur, they can range from mild discomfort to more significant issues.
Pain and Discomfort: When and Why It Happens
If a varicocele causes pain, it is typically described as a dull, aching, or dragging sensation in the scrotum.
The discomfort is not usually sharp or intense. Certain factors can influence the pain:
- Worse with Standing or Exertion: The pain often worsens over the course of the day, especially with prolonged standing, physical activity, or in hot weather. This is because these activities increase blood flow and pressure in the scrotal veins.
- Relieved by Lying Down: Lying on your back allows the pooled blood to drain from the veins, which typically relieves the discomfort.
According to the Urology Care Foundation, while varicoceles can cause pain, it’s important to have a doctor rule out other causes of testicular pain, as the varicocele may not be the source of the discomfort.
Physical Changes: Scrotal Mass and Testicular Size
Beyond the “bag of worms” sensation, a varicocele can cause other noticeable physical changes:
- A Mass in the Scrotum: A large varicocele can present as a visible, non-tender swelling or lump above the testicle.
- Differently Sized Testicles: A varicocele can impair the growth of the affected testicle, a condition known as testicular atrophy or hypotrophy. The affected testicle may be noticeably smaller than the other one. This is a key indicator for considering treatment, especially in adolescents.
The Silent Symptom: Impact on Fertility
Perhaps the most significant complication of a varicocele is its impact on male fertility.
It is the most frequently identified cause of poor sperm production and decreased sperm quality.
According to research published in StatPearls, varicoceles are found in about 40% of men with primary infertility (those who have never fathered a child) and up to 80% of men with secondary infertility (those who have fathered a child previously but are now unable to).
However, it’s crucial to remember that not all varicoceles cause infertility.
Many men with varicoceles have normal fertility and father children without any issues.
When to See a Doctor: Recognizing Warning Signs
It’s important to see a healthcare provider, such as a urologist, if you experience any of the following:
- Pain, swelling, or a lump in your scrotum.
- A noticeable size difference between your testicles.
- You discover a varicocele during a self-exam.
- You and your partner are having difficulty conceiving.
For adolescent boys, annual wellness visits are important for monitoring testicular health and development.
Early detection of a varicocele that is affecting testicular growth can be crucial for preserving future fertility.
What Causes a Varicocele to Develop?
The exact cause of why the valves in the testicular veins fail is not fully understood, but it is widely believed to be related to the anatomy of the male circulatory system.
There do not appear to be any significant lifestyle or genetic risk factors for developing a primary varicocele.
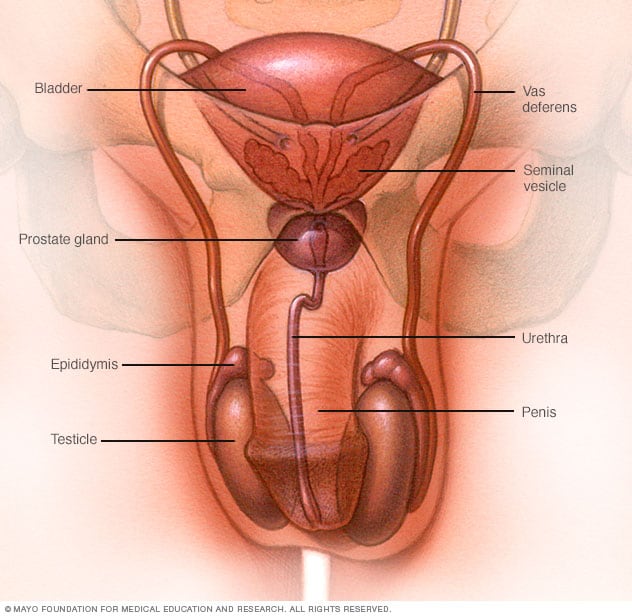
The male reproductive system, where varicoceles form in the veins draining the testicles.
The Anatomy of the Testicular Veins (Left vs. Right)
The overwhelming prevalence of left-sided varicoceles points to an anatomical explanation.
The path of the testicular veins is different on each side of the body:
- The right testicular vein drains directly into the inferior vena cava, a large, low-pressure vein.
- The left testicular vein drains into the left renal (kidney) vein at a sharp 90-degree angle. This connection point is at a higher pressure than the inferior vena cava.
This anatomical arrangement on the left side creates higher pressure in the testicular vein, making it more difficult for blood to drain efficiently.
This increased pressure can overwhelm the one-way valves, leading to their failure and the subsequent formation of a varicocele.
The “Nutcracker Effect” and Other Anatomical Factors
In some cases, a phenomenon known as the “nutcracker effect” (or nutcracker syndrome) can contribute to a varicocele.
This occurs when the left renal vein is compressed between two larger arteries (the superior mesenteric artery and the aorta).
This compression further increases the pressure in the left renal vein and, by extension, the left testicular vein, exacerbating the backflow of blood.
A rare but important consideration is a new, rapidly developing varicocele, especially on the right side or in an older man.
This can sometimes be a sign of a more serious problem, such as a kidney tumor or other mass in the abdomen that is blocking the testicular vein. This is known as a secondary varicocele and requires immediate medical evaluation.
Are There Any Real Risk Factors?
Unlike many medical conditions, there are no well-established risk factors for developing a primary varicocele.
It is not linked to diet, exercise, occupation, or sexual activity.
It appears to be a consequence of human anatomy that affects a random subset of the male population, typically becoming apparent during the rapid growth phase of puberty.
How Does a Varicocele Affect Fertility and Testosterone?
The link between varicocele and male infertility is well-established, though the exact mechanisms are complex and multifactorial.
The pooling of blood in the scrotum disrupts the normal environment of the testicles, leading to several detrimental effects.
The Pathophysiology: How Heat, Hypoxia and Oxidative Stress Damage Sperm
The negative impact of a varicocele on sperm production is thought to be caused by a combination of factors:
- Scrotal Hyperthermia (Increased Temperature): The pampiniform plexus acts as a counter-current heat exchanger, cooling arterial blood before it reaches the testicles. Healthy sperm production (spermatogenesis) requires a temperature about 2-3°C cooler than the core body temperature. The pooled, warm venous blood in a varicocele disrupts this cooling mechanism, raising the scrotal temperature. As confirmed by studies, even a slight increase in temperature can severely impair sperm production and function.
- Oxidative Stress: The stagnant blood in a varicocele is low in oxygen and can contain a buildup of metabolic byproducts. This environment promotes the generation of reactive oxygen species (ROS), leading to a state of oxidative stress. A review in the journal Frontiers in Physiology highlights that high levels of ROS can damage sperm DNA, impair sperm motility and damage the sperm’s cell membrane.
- Testicular Hypoxia (Low Oxygen): The sluggish blood flow reduces the oxygen supply to the testicular tissue, which can further harm sperm development.
- Hormonal Imbalance: A varicocele can affect the function of the Leydig cells in the testicles, which are responsible for producing testosterone. This can lead to lower testosterone levels, which not only impacts fertility but can also cause symptoms like low energy, reduced libido and mood changes.
Varicocele and Infertility by the Numbers
The statistics surrounding varicocele and infertility paint a clear picture of its clinical significance:
- 15-20% of all men have a varicocele.
- ~40% of men evaluated for primary infertility have a varicocele.
- ~80% of men with secondary infertility have a varicocele.
- Treatment of a varicocele can improve semen parameters in 60-80% of men.
How Is a Varicocele Diagnosed?
Diagnosing a varicocele is typically straightforward and involves a combination of a physical examination and imaging studies.
The goal is not just to identify the varicocele but also to determine its size and its impact on testicular health and function.
The Physical Examination: Grading the Varicocele
The gold standard for diagnosis is a physical exam performed by a urologist.
The exam is done with the patient standing in a warm room to relax the scrotal muscles. The doctor will visually inspect and palpate the scrotum.
The patient may be asked to perform the Valsalva maneuver (bearing down as if having a bowel movement).
This increases pressure in the abdomen and makes the varicocele more prominent.
Based on this exam, varicoceles are clinically graded.
| Grade | Description |
|---|---|
| Grade I | Smallest. Palpable (can be felt) only during the Valsalva maneuver. |
| Grade II | Medium. Palpable at rest (without Valsalva), but not visible. |
| Grade III | Largest. Easily visible through the scrotal skin at rest. |
| Subclinical | Not palpable or visible on exam. Detected only by imaging (e.g., ultrasound). Generally, treatment is not recommended for subclinical varicoceles. |
The Role of Scrotal Doppler Ultrasound
A scrotal Doppler ultrasound is a non-invasive imaging test that uses sound waves to create images of the scrotum and assess blood flow.
It is the most reliable tool to confirm the diagnosis and gather objective data.
During the ultrasound, the technician will look for:
- Vein Diameter: The presence of multiple veins in the pampiniform plexus with a diameter greater than 3 millimeters is a key diagnostic criterion.
- Venous Reflux: The Doppler component is crucial. It can detect the backward flow of blood, especially during the Valsalva maneuver. A reversal of flow lasting more than 1-2 seconds is considered pathological.
- Testicular Volume: The ultrasound provides precise measurements of both testicles. A size discrepancy of more than 20% between the affected and unaffected testicle is considered significant and is a strong indication for treatment, particularly in adolescents.
Semen Analysis: Assessing the Functional Impact
For men who are part of a couple struggling with infertility, a semen analysis is essential.
This lab test evaluates the health and viability of a man’s sperm. A varicocele can negatively affect several key parameters:
- Sperm Count (Concentration): The number of sperm per milliliter of semen.
- Sperm Motility: The percentage of sperm that are moving.
- Sperm Morphology: The percentage of sperm that have a normal shape.
A classic finding in men with varicocele-related infertility is the “stress pattern”, characterized by low motility, poor morphology, and a borderline or low sperm count.
Hormonal Blood Tests
In some cases, particularly if there is a significant size difference in the testicles or symptoms of low testosterone, a doctor may order blood tests to check hormone levels, including total and free testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH).
What Are the Treatment Options for a Varicocele?
Not every varicocele needs to be treated. The decision to treat is based on a combination of factors, including the patient’s symptoms, fertility goals and the results of the physical exam and diagnostic tests.
According to joint guidelines from the American Urological Association (AUA) and American Society for Reproductive Medicine (ASRM), indications for treatment generally include:
- A palpable varicocele in a man with documented infertility and abnormal semen parameters.
- Chronic, bothersome scrotal pain attributed to the varicocele.
- In an adolescent, evidence of progressive testicular atrophy.
Conservative Management: When Is “Watchful Waiting” Appropriate?
For men with an asymptomatic varicocele and no fertility concerns, or for adolescents with a small varicocele and no testicular size discrepancy, no immediate treatment is usually necessary. Management may include:
- Pain Relief: For mild, occasional discomfort, over-the-counter pain relievers like ibuprofen or acetaminophen can be helpful. Wearing supportive underwear or an athletic supporter can also alleviate the dragging sensation.
- Monitoring: Adolescents with a varicocele are often monitored with annual physical exams and ultrasounds to track testicular growth.
Surgical Treatment: Varicocelectomy
Varicocelectomy is the surgical repair of a varicocele.
The goal is to ligate (tie off) all the abnormal veins that are allowing blood to flow backward, while preserving the testicular artery, vas deferens (the tube that carries sperm), and lymphatic drainage. Several techniques exist.
Microsurgical Varicocelectomy (Subinguinal/Inguinal): The Gold Standard
This is widely considered the most effective surgical technique with the highest success rates and lowest complication rates. It is performed by a urologist with specialized training in microsurgery.
- Procedure: A small (2-3 cm) incision is made in the groin area (inguinal or subinguinal). A powerful operating microscope is used to provide high magnification, allowing the surgeon to precisely identify and ligate the tiny, dilated veins while carefully sparing the critical arteries and lymphatic vessels.
- Advantages: As documented in numerous urological studies, this technique has the lowest recurrence rate (around 1%) and the lowest risk of complications like hydrocele (fluid buildup around the testicle) and testicular artery injury.
Laparoscopic Varicocelectomy
This technique involves making several small incisions in the abdomen.
A camera (laparoscope) and surgical instruments are inserted to identify and clip the testicular veins higher up in the abdomen.
While it allows for the treatment of bilateral (both sides) varicoceles through the same incisions, it is generally associated with higher recurrence rates and a greater risk of intra-abdominal complications compared to the microsurgical approach.
Minimally Invasive Treatment: Varicocele Embolization
Varicocele embolization is a non-surgical, minimally invasive procedure performed by an interventional radiologist. It is an effective alternative to surgery for many patients.
- Procedure: A small catheter is inserted into a vein, typically in the groin or neck. Using X-ray guidance, the radiologist navigates the catheter to the problematic testicular vein. Small metal coils, a glue-like substance, or a sclerosing agent are then deployed to block the vein. This stops the backflow of blood, and the body naturally reroutes blood flow through healthy veins.
- Advantages: It is an outpatient procedure, usually performed with local anesthesia and light sedation. There is no surgical incision in the scrotum or groin, recovery is very quick (often returning to normal activities in 1-2 days) and the risk of hydrocele is very low.
- Disadvantages: It has a slightly higher recurrence rate than microsurgery (around 4-11%). There is also a small risk of technical failure, where the radiologist cannot access the target vein.
Table: Comparing Varicocele Treatment Options
| Feature | Microsurgical Varicocelectomy | Varicocele Embolization |
|---|---|---|
| Procedure Type | Surgical | Minimally Invasive, Radiological |
| Anesthesia | General or Spinal | Local with Sedation |
| Success Rate | ~98% | ~90-95% |
| Recurrence Rate | ~1% (Lowest) | ~4-11% |
| Recovery Time | 1-2 weeks for full activity | 1-2 days for full activity |
| Key Risks | Infection, hydrocele, arterial injury (all rare with microsurgery) | Coil migration, vein perforation, contrast allergy (all rare) |
| Best For | Considered the “gold standard” for fertility; best for bilateral repair | Patients wanting to avoid surgery; treatment of recurrence after surgery |
What Is the Recovery and Outlook After Varicocele Treatment?
The prognosis after varicocele repair is generally excellent, both for symptom relief and for improving fertility potential.
Recovery Timeline: What to Expect
- After Embolization: Recovery is very fast. Most patients can return to work and light activities within 24-48 hours. Strenuous exercise can usually be resumed within a week. Mild pain or discomfort may be managed with over-the-counter medication.
- After Microsurgery: Recovery is slightly longer. Patients are advised to avoid heavy lifting and strenuous activity for 1-2 weeks. Scrotal support is recommended. Pain is typically mild and well-controlled with prescribed medication for a few days.
Impact on Semen Parameters: How Soon Do Sperm Improve?
One of the most common questions from patients is how long it takes to see an improvement in sperm quality.
The process of spermatogenesis (the full cycle of sperm production) takes approximately 72-90 days.
A key study published in the Journal of Urology found that sperm parameters significantly improve by 3 months after varicocele repair and then typically plateau, with little further improvement after 6 months.
This means that a follow-up semen analysis is usually performed 3 to 6 months after the procedure to assess its effectiveness.
Significant improvements in sperm count, motility, and morphology are seen in 60-80% of men who undergo treatment.
Pregnancy Rates After Treatment: Natural and Assisted
The ultimate goal of varicocele repair for infertility is to achieve a pregnancy.
Studies have shown that treatment significantly improves pregnancy rates.
- Natural Conception: A Cochrane Review, a high-level analysis of medical research, found that varicocele treatment in men from couples with unexplained subfertility can improve the chances of natural conception. Spontaneous pregnancy rates after varicocelectomy are reported to be between 30% and 60%.
- Assisted Reproductive Technology (ART): For couples who still require ART (like IVF or ICSI) after varicocele repair, the procedure may still be beneficial. It can “upgrade” a couple from needing a more invasive procedure like ICSI to a less invasive one like IUI, or improve the outcomes of IVF/ICSI cycles.
Long-Term Prognosis and Recurrence
The long-term outlook is very good. For men with pain, over 90% experience significant or complete resolution of their symptoms after repair.
Recurrence is the main long-term concern, but with modern techniques like microsurgery, the risk is very low.
If a varicocele does recur, it can often be effectively treated with embolization.
Varicocele in Adolescents: A Special Consideration
The management of varicocele in adolescents is a distinct and sometimes controversial topic.
Since fertility is not an immediate concern, the primary focus is on preventing future problems.
Why It’s Different in Teenagers
In adolescents, a varicocele can interfere with the normal growth and development of the testicle during the crucial period of puberty.
The main concern is the development of testicular hypotrophy (impaired growth), which can be a predictor of future fertility problems.
Indications for Treatment in Adolescents
According to guidelines from pediatric urology experts, surgery is generally recommended for an adolescent with a varicocele if they have one or more of the following:
- Significant Testicular Size Discrepancy: A volume difference of more than 20% compared to the other testicle. This is the most common indication.
- Bothersome Pain: Persistent pain that interferes with daily activities.
- Abnormal Hormone Levels: Though less common, this can be a factor.
- Abnormal Semen Analysis: If obtainable in an older adolescent.
The Debate: Treat or Observe?
For adolescents who have a varicocele but normal testicular size, the standard approach is observation with annual follow-up exams.
The debate centers on whether to treat proactively to prevent any potential future decline in function or to wait until a problem (like testicular atrophy or abnormal semen parameters) arises.
The decision is highly individualized and made after a thorough discussion between the urologist, the patient and their parents.
Frequently Asked Questions (FAQ) about Varicocele
1. Can a varicocele go away on its own?
No, a varicocele is a physical abnormality of the veins and will not resolve on its own. While symptoms may fluctuate, the underlying condition of dilated veins will persist unless treated with surgery or embolization.
2. Is a varicocele dangerous?
A varicocele is not life-threatening. Its main risks are related to testicular health, including potential pain, testicular atrophy (shrinkage), and impaired fertility. A sudden, painful varicocele, especially on the right side, could indicate a more serious issue and requires immediate medical attention.
3. Can exercise make a varicocele worse?
Exercise does not cause a varicocele, but activities that increase intra-abdominal pressure (like heavy weightlifting) can temporarily make it more prominent and may worsen symptoms of aching or discomfort. It does not, however, worsen the underlying condition itself.
4. Does a varicocele always cause infertility?
No. While it is a leading cause of male infertility, many men with a varicocele have normal fertility and can father children without any medical intervention. Treatment is only recommended for infertility when a palpable varicocele is present alongside abnormal semen parameters.
5. Is varicocele treatment painful?
Modern treatment methods are designed to minimize pain. Embolization involves only a tiny skin nick and has a very quick recovery. Microsurgery involves a small incision, and postoperative pain is typically mild and well-managed with medication for a few days.
6. Which side is more common for a varicocele?
The left side is far more common, accounting for about 80-90% of all cases. This is due to the anatomy of the left testicular vein, which joins the left renal vein at a higher pressure point, making it harder for blood to drain.
7. Can I have a child if I have a varicocele?
Yes, absolutely. Many men with varicoceles father children naturally. If you have a varicocele and are struggling to conceive, treatment can significantly improve your chances. A consultation with a urologist is the best way to assess your individual situation.
8. What is a “subclinical” varicocele?
A subclinical varicocele is one that is too small to be felt or seen during a physical exam but is detected on an imaging test like an ultrasound. Major urological and reproductive societies do not recommend treating subclinical varicoceles for infertility.
Conclusion
A varicocele is a common and highly manageable condition. While it is a leading correctable cause of male infertility and can cause discomfort, it is not a life-threatening issue.
For many, it requires no treatment at all. For those affected by pain or fertility problems, modern medicine offers highly effective and safe treatment options, from state-of-the-art microsurgery to minimally invasive embolization.
Knowledge is power. Understanding the symptoms, causes, and treatments for varicocele allows you to make informed decisions about your health.
If you suspect you have a varicocele or are concerned about your fertility, the most important step is to consult with a urologist for an accurate diagnosis and a personalized treatment plan tailored to your specific needs and goals.
We hope this guide has provided you with the clarity and confidence to address this condition.
Do you have an experience with varicocele or a question we didn’t cover? Share your thoughts in the comments below to help others in the community.
Medical Disclaimer
The information provided in this article is for educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.