The primary symptom of kidney stones is severe, sharp pain in your back, side, lower abdomen, or groin, often accompanied by blood in the urine.
This condition, known medically as nephrolithiasis, affects an estimated 1 in 11 people in the United States during their lifetime, with prevalence rates showing a significant increase over the past few decades.
While some tiny kidney stones may pass without you ever knowing, others can cause excruciating pain that some women have described as worse than childbirth.
Understanding the key symptoms is crucial for seeking timely medical care and preventing potential complications.
This comprehensive guide will walk you through the five most critical signs of kidney stones, explain what causes them, how they are diagnosed, and what you can do for treatment and prevention.
In This Article
Symptom 1: Severe, Sharp Pain (Renal Colic)
The hallmark symptom of kidney stones is a sudden, excruciating pain known as renal colic.
This isn’t a dull ache, it’s a severe, sharp and often cramping pain that can be debilitating.
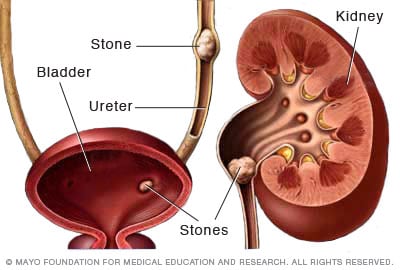
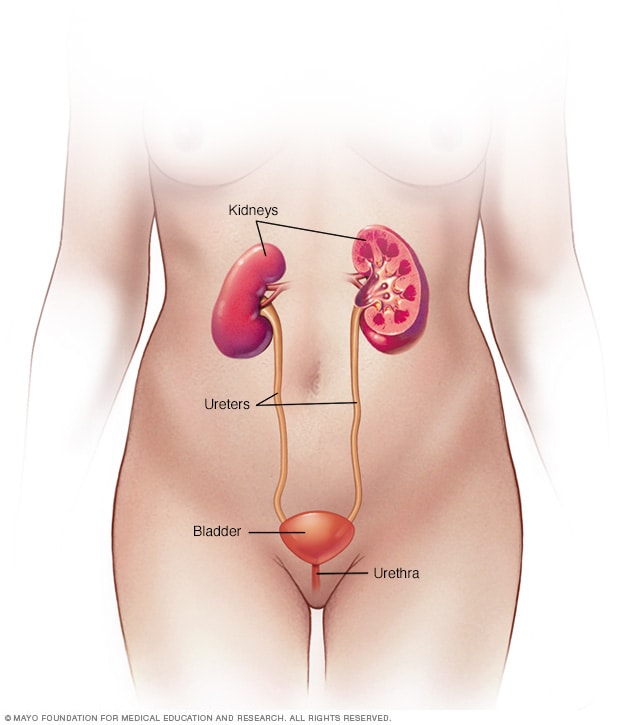
The pain begins when a stone moves from the kidney into the narrow ureter, the tube that carries urine to the bladder.
This movement can block the flow of urine, causing the kidney to swell (a condition called hydronephrosis) and the ureter to spasm.
This combination of pressure and spasm is what generates the intense pain.
According to the American Urological Association (AUA), many female patients describe the pain as more intense than childbirth.
Characteristics of Renal Colic:
- Location of Pain: The pain typically starts in the side and back, just below the ribs (the flank area). As the stone moves down the ureter, the pain often radiates to the lower abdomen and groin.
- Pain That Comes in Waves: Renal colic is often described as coming in waves, fluctuating in intensity. These waves correspond to the ureter’s peristaltic movements as it tries to push the stone along.
- Inability to Get Comfortable: A key feature that distinguishes kidney stone pain is the patient’s restlessness. People with renal colic are often seen writhing in pain, constantly moving to find a comfortable position, but failing to do so. This is in contrast to pain from conditions like appendicitis, where movement makes the pain worse.
- Pain During Urination (Dysuria): As the stone nears the bladder, it can cause a sharp, burning pain during urination. This can sometimes be mistaken for a urinary tract infection (UTI).
Expert Insight: The pain from kidney stones is not caused by the stone itself being “sharp”, but by the obstruction it creates. The buildup of pressure behind the stone stretches the kidney and ureter, which are rich in nerve endings, leading to the severe pain signals sent to the brain.
Symptom 2: Changes in Urination
As a kidney stone makes its journey through your urinary tract, it can cause a host of noticeable changes in your urination patterns.
These symptoms often become more pronounced as the stone moves closer to the bladder, at the ureterovesical junction.
Common Urinary Symptoms:
- Persistent Urge to Urinate (Urgency): You might feel a constant, strong need to go to the bathroom, even if you’ve just urinated. This is due to the stone irritating the lower part of the ureter and the bladder itself.
- Frequent Urination (Frequency): You may find yourself needing to urinate more often than usual, but often only passing small amounts of urine each time.
- Cloudy or Foul-Smelling Urine: The presence of crystals, pus, or bacteria can make urine appear cloudy. A strong, foul odor can be a sign of a secondary infection, which is a serious complication of kidney stones.
- Difficulty Passing Urine: In some cases, a large stone can partially or fully block the urethra, making it difficult to start or maintain a urine stream. This is a medical emergency that requires immediate attention.
These urinary symptoms can easily be confused with a urinary tract infection (UTI).
In fact, UTIs can sometimes occur alongside kidney stones, especially with a type of stone called a struvite stone.
It’s essential to get a proper diagnosis from a healthcare professional.
Symptom 3: Blood in the Urine (Hematuria)
Seeing blood in your urine can be alarming, but it’s a very common sign of kidney stones.
The medical term for this is hematuria. It occurs when the stone scrapes against the delicate lining of the kidney or ureter, causing it to bleed.
How Hematuria Presents:
- Gross Hematuria: This is when the blood is visible to the naked eye. Your urine may appear pink, red or brown (like cola).
- Microscopic Hematuria: Sometimes, the amount of blood is so small that it can only be detected with a microscope during a urinalysis. You might have no idea it’s there.
According to a study published in the Endotext, hematuria (either gross or microscopic) is present in a large majority of patients with renal colic.
However, its absence does not rule out kidney stones.
It’s possible to have a stone without any visible or microscopic blood in the urine.
“While hematuria is a classic sign, its absence should not dissuade a clinician from the diagnosis of urolithiasis in a patient with a typical presentation of flank pain.”
Symptom 4: Nausea and Vomiting
The intense pain of renal colic can often trigger nausea and vomiting.
This is a systemic response to severe pain and is not unique to kidney stones, but it is a very common accompanying symptom.
The connection between the kidneys and the gastrointestinal (GI) tract is through shared nerve pathways.
When the nerves in the kidney and ureter are overstimulated by the pain of a passing stone, they can send signals that upset the GI tract, leading to feelings of nausea and the physical act of vomiting.
This symptom can be particularly problematic because vomiting can lead to dehydration.
Dehydration, in turn, makes the urine more concentrated, which can worsen the conditions that form kidney stones in the first place. It can also make it harder for a stone to pass.
If you are unable to keep fluids down due to persistent vomiting, it’s crucial to seek medical help to prevent dehydration.
Symptom 5: Fever and Chills
Fever and chills are not typical symptoms of an uncomplicated kidney stone.
When they appear alongside kidney stone pain, it is a major red flag.
This combination strongly suggests that you have an infection in your urinary tract that is being complicated by the stone’s blockage.
When a stone obstructs the flow of urine, it creates a stagnant pool of urine behind it.
This is an ideal breeding ground for bacteria. If an infection takes hold, it can quickly become serious, leading to a condition called pyelonephritis (a kidney infection) or even urosepsis, a life-threatening infection that has spread to the bloodstream.
CRITICAL WARNING: If you experience severe flank pain accompanied by a fever (typically over 100.4°F or 38°C) and chills, this is a medical emergency. You should go to the nearest emergency room immediately.
An infected, obstructed kidney requires urgent medical intervention to drain the urine and treat the infection with antibiotics, often intravenously.
Delaying treatment can lead to permanent kidney damage or a life-threatening systemic infection.
When Should You See a Doctor for Kidney Stone Pain?
While some small kidney stones can be managed at home with pain medication and increased fluid intake, certain symptoms warrant immediate medical attention.
According to the Mayo Clinic, you should seek immediate medical care if you experience:
- Pain so severe that you can’t sit still or find a comfortable position.
- Pain accompanied by nausea and vomiting that prevents you from keeping fluids down.
- Pain accompanied by fever and chills.
- Visible blood in your urine.
- Difficulty passing urine or a complete inability to urinate.
Even if your pain is manageable, it’s always a good idea to make an appointment with your healthcare professional to confirm the diagnosis and create a management plan.
A proper diagnosis is essential to rule out other serious conditions that can mimic kidney stone pain, such as appendicitis, ovarian cysts, or an aortic aneurysm.
What Exactly Are Kidney Stones?
A kidney stone is a hard, solid, pebble-like object that forms inside the kidneys.
They are created from minerals and salts that crystallize out of the urine.
These stones can vary dramatically in size, from as small as a grain of sand to as large as a golf ball.
Other names for this condition include renal calculi, nephrolithiasis or urolithiasis.
The urinary system is designed to filter waste from the blood and excrete it as urine.
This system includes the kidneys, ureters, bladder and urethra.
Kidney stones can form in the kidneys and may travel through, and potentially get stuck in, any part of this tract.
The fundamental cause of stone formation is a state of supersaturation in the urine.
This occurs when the urine contains more crystal-forming substances (like calcium, oxalate and uric acid) than the fluid in the urine can dilute.
At the same time, the urine may lack substances that naturally prevent crystals from sticking together, creating the perfect environment for kidney stones to form.
What Causes Kidney Stones and Who Is at Risk?
There is often no single, definitive cause for kidney stones. Instead, a combination of genetic, environmental, dietary and medical factors contribute to an individual’s risk.
The lifetime prevalence of kidney stones has been steadily increasing, with data from the National Health and Nutrition Examination Survey (NHANES) showing a rise from 3.8% in the late 1970s to over 10% in recent years, as reported in a 2023 study in Epidemiology of Kidney Stones.
Major Risk Factors Include:
- Dehydration: Not drinking enough water is the single most common cause of kidney stones. Low fluid intake leads to concentrated urine, increasing the chances of crystal formation.
- Diet: Diets high in sodium, sugar and animal protein can increase the risk. High sodium intake, in particular, increases the amount of calcium your kidneys must filter, raising the risk of calcium stones. Certain foods high in oxalate (like spinach, nuts and chocolate) can also contribute, especially in susceptible individuals.
- Family or Personal History: If you’ve had a kidney stone before, your risk of having another is about 50% within the next 10 years. A family history also significantly increases your risk.
- Obesity: Having a high body mass index (BMI) is strongly linked to an increased risk of kidney stones.
- Medical Conditions: Certain health issues increase risk, including recurrent urinary tract infections (UTIs), hyperparathyroidism (an overactive parathyroid gland), renal tubular acidosis and genetic conditions like cystinuria.
- Digestive Diseases and Surgery: Conditions like inflammatory bowel disease (IBD), chronic diarrhea, or gastric bypass surgery can alter the digestive process, affecting the absorption of calcium and water and increasing stone-forming substances in the urine.
- Medications and Supplements: Certain medications, such as some diuretics, calcium-based antacids, and the anti-seizure drug topiramate, can increase the risk. High doses of vitamin C supplements have also been linked to stone formation.
What Are the Different Types of Kidney Stones?
Knowing the type of kidney stone you have is crucial because it helps your doctor determine the underlying cause and tailor a specific prevention plan.
If you pass a stone, your doctor will likely ask you to retrieve it for analysis. There are four main types of kidney stones.

| Stone Type | Prevalence | Primary Cause(s) | Key Characteristics |
|---|---|---|---|
| Calcium Oxalate | ~80% | High oxalate in urine, high calcium in urine, low urine volume. Often linked to diet and dehydration. | Most common type. Can be caused by dietary factors, high doses of vitamin D or metabolic disorders. |
| Uric Acid | 5-10% | High-protein diet, gout, chronic diarrhea, genetic factors, acidic urine (low pH). | More common in men. Can sometimes be dissolved with medication that makes urine more alkaline. |
| Struvite | 5-10% | Chronic urinary tract infections (UTIs) caused by specific urease-producing bacteria. | Often called “infection stones”. Can grow very large, sometimes filling the entire kidney (staghorn calculus), and can form quickly with few symptoms. More common in women. |
| Cystine | ~1% | A rare, inherited genetic disorder called cystinuria, which causes the amino acid cystine to leak into the urine. | These stones are caused by a hereditary condition and often begin to form in childhood. They can be difficult to treat and tend to recur frequently. |
How Are Kidney Stones Diagnosed?
Diagnosing kidney stones involves a combination of reviewing your symptoms and medical history, a physical exam and specific diagnostic tests.
The goal is not only to confirm the presence of a stone but also to determine its size, location and whether it’s causing an obstruction.
Common Diagnostic Tests:
- Blood Tests: These can reveal high levels of calcium or uric acid in your blood, which can point to the underlying cause of your kidney stones. Blood tests also check your kidney function.
- Urine Tests: A urinalysis can detect blood, white blood cells (a sign of infection) and crystals. A 24-hour urine collection test is more comprehensive, it measures the volume of your urine and the levels of stone-forming and stone-inhibiting substances over a full day. This test is invaluable for creating a long-term prevention plan.
- Imaging Tests: This is the definitive way to diagnose a kidney stone.
- Computed Tomography (CT) Scan: A non-contrast helical CT scan is considered the “gold standard” for diagnosing kidney stones. It is highly sensitive and specific, able to detect stones of all types and sizes, and can clearly show if the stone is causing a blockage.
- Ultrasound: This is a non-invasive test that uses sound waves to create images. It does not use radiation, making it the preferred first-line test for pregnant women and children. While good at detecting stones in the kidney and significant blockages, it is less effective at seeing smaller stones in the ureter.
- X-ray (KUB): A kidney-ureter-bladder (KUB) X-ray can see some types of stones (especially calcium stones) but can miss others (like uric acid stones). It is used less often for initial diagnosis but can be useful for monitoring the growth of a known stone over time due to its lower radiation exposure compared to a CT scan.
- Analysis of Passed Stones: If you pass a stone, your doctor will ask you to collect it using a strainer. Analyzing the stone’s chemical composition is the most accurate way to determine its type and guide prevention strategies.
Expert Insight: While a CT scan is the most accurate diagnostic tool, a 2024 report from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) highlights that it remains the predominant imaging modality, with 70% of patients undergoing a CT scan around the time of their diagnosis. This underscores its importance in modern urological practice.
What Are the Treatment Options for Kidney Stones?
Treatment for kidney stones depends on the stone’s type, size, location and the severity of your symptoms.
Small stones may pass on their own, while larger or more problematic stones require active intervention.
Conservative Management (for Small Stones)
For small stones (typically less than 5 mm) that are not causing severe pain, infection, or blockage, your doctor may recommend a “watch and wait” approach.
- Hydration: Drinking plenty of water (2-3 liters per day) helps flush the urinary system and can help the stone pass.
- Pain Relief: Over-the-counter pain relievers like ibuprofen or naproxen sodium can help manage discomfort.
- Medical Expulsive Therapy (MET): Your doctor may prescribe a medication called an alpha-blocker (such as tamsulosin). This drug relaxes the muscles in the ureter, making it easier for the stone to pass.
Surgical and Procedural Interventions (for Large or Problematic Stones)
When a stone is too large to pass, causes unbearable pain, blocks urine flow, or is associated with an infection, more invasive treatment is necessary.
- Extracorporeal Shock Wave Lithotripsy (ESWL): This is a non-invasive procedure that uses high-energy sound waves to break the kidney stone into tiny, sand-like particles that can then be passed in the urine. It is most effective for stones located in the kidney or upper ureter.
- Ureteroscopy (URS): A surgeon inserts a very thin, lighted tube (a ureteroscope) through the urethra and bladder into the ureter. Once the stone is located, it can be removed with a small basket or broken up with a laser. This procedure is highly effective for stones in the mid to lower ureter.
- Percutaneous Nephrolithotomy (PCNL): This is a more invasive procedure reserved for very large or complex kidney stones (e.g., staghorn calculi). A surgeon makes a small incision in the back and creates a tunnel directly into the kidney. A nephroscope is used to locate and remove the stone or break it apart.
The choice of procedure is a shared decision between you and your urologist, based on the specific characteristics of your stone and your overall health.
How Can You Prevent Future Kidney Stones?
After experiencing the pain of a kidney stone, most people are highly motivated to prevent another one.
Prevention strategies are highly effective and are tailored to the type of stone you form.
General Lifestyle Changes for All Stone Formers:
- Increase Fluid Intake: This is the single most important preventive measure. The AUA guidelines recommend drinking enough fluid to produce at least 2.5 liters of urine per day. Water is best. Your urine should be light yellow or clear.
- Dietary Modifications:
- Reduce Sodium: Limit processed foods, fast food, and canned soups. A high-sodium diet increases calcium in your urine.
- Moderate Animal Protein: Reduce intake of red meat, poultry and fish, as they can increase uric acid and decrease citrate levels.
Specific Prevention Based on Stone Type:
- For Calcium Oxalate Stones: In addition to general advice, you may need to limit high-oxalate foods like spinach, rhubarb, beets, nuts and tea. It’s important to consume a normal amount of dietary calcium (from food, not supplements). Paradoxically, a low-calcium diet can actually increase your risk of forming these stones.
- For Uric Acid Stones: Limit high-purine foods like organ meats, shellfish and red meat. Your doctor may also prescribe a medication like allopurinol to lower uric acid levels or potassium citrate to make your urine less acidic.
- For Struvite Stones: The key is to prevent UTIs. This may involve long-term, low-dose antibiotics in some rare cases.
- For Cystine Stones: This requires a specialized plan that includes very high fluid intake and medications to make the urine more alkaline.
Working with a healthcare professional or a registered dietitian specializing in kidney disease can help you create a personalized and effective prevention plan.
Frequently Asked Questions (FAQ)
1. How long does it take to pass a kidney stone?
The time varies greatly depending on size and location. Stones smaller than 4 mm often pass within 1-2 weeks, while larger stones (over 6 mm) may take a month or longer and are more likely to require medical intervention.
2. Can kidney stones cause permanent damage?
If treated promptly, kidney stones rarely cause permanent damage. However, a stone causing a prolonged blockage or a severe infection can lead to chronic kidney disease or loss of kidney function if not addressed urgently.
3. What is the best thing to drink to flush out kidney stones?
Water is the best fluid for flushing out kidney stones. Aim for 2-3 liters per day. Some evidence suggests that drinks high in citrate, like lemon juice mixed with water, may also help by preventing calcium stones from forming.
4. Do I need to avoid calcium if I have calcium kidney stones?
No, this is a common misconception. Eating a normal amount of calcium from food sources can actually help prevent calcium oxalate stones. However, you should talk to your doctor before taking calcium supplements, as they have been linked to an increased risk.
5. Can stress cause kidney stones?
While stress itself doesn’t directly form stones, it can lead to behaviors that increase your risk, such as poor dietary choices, dehydration, or not taking prescribed medications. Managing stress is part of a healthy lifestyle that can help prevent stones.
6. Are men more likely to get kidney stones than women?
Historically, men have had a higher incidence. However, recent data from the Epidemiology of Kidney Stones review shows this gap is narrowing, with prevalence increasing more rapidly in women. The lifetime risk is now estimated at about 1 in 8 for men and 1 in 11 for women.
7. Can children get kidney stones?
Yes, although less common than in adults, the incidence of kidney stones in children is rising. The causes are often related to diet, dehydration and sometimes underlying metabolic or anatomical abnormalities. Any child with a stone requires a full metabolic workup.
8. What does kidney stone pain feel like?
It’s typically a severe, sharp, cramping pain in the back or side that comes in waves and may radiate to the groin. Patients often cannot find a comfortable position and may experience nausea, vomiting and blood in the urine.
Conclusion
Kidney stones are a common and incredibly painful condition, but they are also highly manageable and, in many cases, preventable.
Recognizing the top five symptoms—severe pain, urinary changes, blood in the urine, nausea/vomiting, and fever/chills—is the first and most critical step toward getting the right diagnosis and treatment.
Never ignore severe pain, especially when accompanied by fever.
Modern diagnostics can quickly identify the problem, and a range of effective treatments, from simple hydration to advanced surgical procedures, can provide relief.
Most importantly, by understanding your specific risk factors and stone type, you can make powerful lifestyle and dietary changes to significantly reduce your chances of ever forming another stone.
We hope this guide has empowered you with the knowledge to understand and address kidney stones.
If you have experienced these symptoms or have further questions, we encourage you to consult a healthcare professional.
Please share this article with anyone who might benefit from this information.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. The information contained herein is not a substitute for, and should never be relied upon for, professional medical advice. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.

