Allergies are a chronic condition caused by an overreaction of the immune system to normally harmless substances, known as allergens.
This misguided defensive response triggers a cascade of chemical releases in the body, leading to a wide spectrum of symptoms that can range from mildly irritating to life-threatening.
The impact of allergies on public health is staggering. According to data from the Centers for Disease Control and Prevention (CDC), more than a quarter of U.S. adults and children—representing over 100 million people—suffer from at least one allergy.
As reported by the American College of Allergy, Asthma and Immunology (ACAAI), allergies are the 6th leading cause of chronic illness in the United States, underscoring their profound effect on daily life, productivity and healthcare costs.
This guide is designed to be your definitive resource for navigating the complex world of allergies.
We will embark on a comprehensive journey, starting with the fundamental science of what happens inside your body during an allergic reaction.
We will then explore how to identify the diverse types of allergies and their specific symptoms, delve into modern diagnostic tests that provide clarity, and finally, navigate the full spectrum of treatment and management strategies available today.
By the end of this article, you will be equipped with the knowledge to better understand, manage and take control of your allergies.
In This Articles
The Fundamental Science of an Allergic Reaction
What Exactly Are Allergies? The Science Explained
At its core, an allergy is a case of mistaken identity on a microscopic scale.
Your immune system is a highly sophisticated and vigilant network of cells, tissues and organs designed to be your body’s primary defense force.
Its main purpose is to identify and neutralize genuine threats, such as viruses, bacteria and other pathogens.
In most individuals, this system works flawlessly, distinguishing between harmful invaders and benign substances from the environment.
However, in a person with allergies, this system makes a critical error. It incorrectly flags a normally harmless substance—an allergen—as a dangerous intruder.
This could be anything from a grain of pollen to a protein in peanuts. This initial misidentification sets off a chain reaction that defines the allergic response.
The Key Players in an Allergic Reaction
To understand the process, it’s essential to know the key players involved:
- The Allergen: This is the trigger substance. Common allergens include pollen, dust mites, mold spores, pet dander, certain foods, insect venom and some medications.
- Immunoglobulin E (IgE): Think of this as the “allergy antibody”. When a person prone to allergies is first exposed to an allergen, their immune system doesn’t typically have a major reaction. Instead, it quietly produces a large quantity of specific IgE antibodies tailored to that exact allergen. This initial process is called sensitization. These IgE antibodies then circulate through the bloodstream.
- Mast Cells and Basophils: These are specialized immune cells found in tissues throughout the body, particularly in areas that are common entry points for allergens, like the skin, nose, lungs and digestive tract. The IgE antibodies produced during sensitization attach themselves to the surface of these mast cells and basophils, effectively arming them and putting them on high alert.
- Histamine and Other Chemical Mediators: Mast cells are like tiny grenades packed with powerful inflammatory chemicals. The most well-known of these is histamine, but they also contain leukotrienes, prostaglandins and cytokines.
The Two-Step Process: Sensitization and Reaction
The allergic response unfolds in two distinct phases:
Phase 1: Sensitization. The first time you encounter a potential allergen, like ragweed pollen, your body may not show any outward symptoms.
Internally, however, your immune system is busy. It processes the pollen, deems it a threat, and B-cells (a type of white blood cell) begin producing specific IgE antibodies against it.
These antibodies then attach to mast cells, where they lie in wait. You are now “sensitized” to ragweed pollen, but you wouldn’t know it yet.
Phase 2: The Allergic Reaction. The next time you are exposed to the same allergen—perhaps the following allergy season—the ragweed pollen enters your body and binds to the specific IgE antibodies already coating your mast cells.
This connection acts like a key turning a lock, instantly triggering the mast cells to “degranulate”.
This means they burst open and release their payload of histamine and other chemical mediators into the surrounding tissues.
Imagine your immune system as a highly advanced home security system. In a non-allergic person, the alarm only sounds for a genuine break-in (a virus). In an allergic person, the system has been incorrectly programmed. It now treats the daily mail carrier (pollen) as a dangerous intruder, sounding a full-scale alarm every time they approach. Histamine is the blaring siren and flashing lights of that alarm.
It is this flood of histamine and other chemicals that causes the classic symptoms of an allergy.
Histamine causes blood vessels to dilate and become more permeable (leaky), leading to swelling, redness and fluid buildup.
It stimulates nerves, causing itching. It increases mucus production, resulting in a runny nose and postnasal drip.
It can cause smooth muscles in the airways to constrict, leading to wheezing and shortness of breath.
The specific symptoms you experience depend entirely on where in the body these mast cells are activated.
Identifying the Signs – Symptoms and Types
What Are the Most Common Allergy Symptoms?
Allergy symptoms are the direct result of the chemical mediators, like histamine, being released in different parts of the body.
The location of the reaction determines the signs you’ll experience.
Understanding these symptoms is the first step toward identifying a potential allergy.
Symptoms can be highly specific or generalized, and their severity can range from a minor nuisance to a life-threatening emergency.
Respiratory System (Allergic Rhinitis / Hay Fever)
When allergens are inhaled, they trigger a reaction in the nose, sinuses and throat.
This is commonly known as allergic rhinitis or, more colloquially, hay fever.
- Sneezing: Often in rapid, successive bursts.
- Runny or Stuffy Nose (Congestion): A clear, watery discharge is typical of allergies, distinguishing it from the often thicker, colored mucus of an infection.
- Itchy Nose, Throat, or Roof of Mouth: A persistent, tickling sensation that is a hallmark of an allergic response.
- Watery, Itchy, Red Eyes (Allergic Conjunctivitis): The eyes are often involved, leading to redness, intense itching, and excessive tearing.
- Postnasal Drip and Cough: Excess mucus dripping down the back of the throat can cause irritation and a chronic, dry cough.
- Sinus Pressure and Facial Pain: Chronic congestion can lead to pressure and a feeling of fullness in the forehead and cheeks.
Skin (Dermatitis)
When an allergen comes into contact with the skin or is ingested, it can cause a variety of skin reactions.
- Hives (Urticaria): Itchy, raised, red or skin-colored welts that can appear anywhere on the body. They can vary in size and may appear and fade over several hours.
- Eczema (Atopic Dermatitis) Flare-ups: For individuals with this underlying condition, exposure to allergens can trigger patches of red, itchy, dry and scaly skin.
- Contact Dermatitis: A localized rash caused by direct contact with an allergen, such as nickel in jewelry, latex, or the oil in poison ivy. It often results in redness, itching, bumps and sometimes blisters.
- Swelling (Angioedema): A deeper swelling within the skin, most commonly affecting the lips, eyes, hands, feet or throat. Unlike hives, it is typically not itchy but can be painful.
Digestive System (Food Allergies)
When a food allergen is consumed, the immune reaction is centered in the gastrointestinal tract, though symptoms can also appear elsewhere on the body.
- Tingling or Itching in the Mouth: This is often the very first symptom and can occur within minutes of eating the trigger food.
- Abdominal Pain, Cramps, Nausea, Vomiting or Diarrhea: The body’s attempt to expel the allergen can lead to significant gastrointestinal distress.
- Swelling of the Lips, Tongue or Throat: This is a form of angioedema and can be a sign of a more severe reaction.
Systemic Reaction (Anaphylaxis)
Anaphylaxis is a severe, life-threatening, whole-body allergic reaction that is a medical emergency.
It occurs when the allergic response is so massive that it affects multiple body systems simultaneously.
It can progress rapidly and be fatal if not treated immediately.
Key signs of anaphylaxis include any combination of the above symptoms, plus:
- Difficulty Breathing or Wheezing: Caused by swelling of the throat (laryngeal edema) or constriction of the airways (bronchospasm).
- A Sharp Drop in Blood Pressure (Hypotension): This can lead to dizziness, lightheadedness, a weak and rapid pulse, or loss of consciousness (fainting).
- A Sense of Impending Doom: Many people experiencing anaphylaxis report a sudden feeling of intense anxiety or that something is terribly wrong.
- Skin Symptoms: Widespread hives, flushing, or paleness are common.
- Gastrointestinal Symptoms: Severe cramps, vomiting, or diarrhea can also occur.
Anaphylaxis is most commonly triggered by food allergies, insect stings, medications and latex.
Immediate administration of epinephrine and a call to emergency services (911) are critical.
What Causes Different Types of Allergies?
Allergies are categorized based on their triggers.
While the underlying immune mechanism is the same, the source of the allergen and the route of exposure determine the type of allergy and the typical symptoms experienced.
Environmental & Seasonal Allergies
These are among the most common allergies, triggered by airborne substances.
They are often divided into two categories:
- Seasonal Allergies: These occur at specific times of the year when certain plants are pollinating. Common triggers include tree pollen (spring), grass pollen (late spring and summer), and weed pollen, like ragweed (late summer and fall).
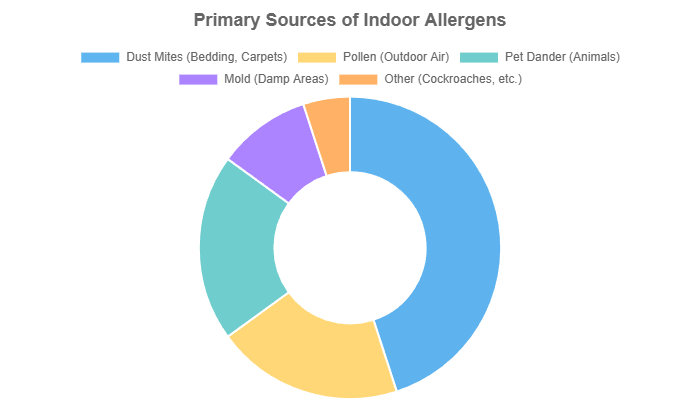
- Perennial Allergies: These occur year-round and are caused by indoor allergens. The primary culprits are dust mites (microscopic creatures that live in bedding, upholstery, and carpets), pet dander (tiny flecks of skin shed by cats, dogs, and other animals with fur or feathers), mold spores (from damp areas like basements and bathrooms), and cockroach droppings.
Food Allergies
A food allergy is an immune system response to a specific protein in a food.
While any food can potentially cause an allergy, the U.S. Food and Drug Administration (FDA) recognizes nine major food allergens that account for over 90% of all reactions:
- Milk
- Eggs
- Fish
- Crustacean shellfish (e.g., shrimp, crab, lobster)
- Tree nuts (e.g., almonds, walnuts, pecans)
- Peanuts
- Wheat
- Soybeans
- Sesame
It is crucial to distinguish a true food allergy from a food intolerance.
A food intolerance, such as lactose intolerance, does not involve the immune system.
It is typically a digestive issue caused by the body’s inability to break down a certain food component (e.g., a lack of the lactase enzyme to digest milk sugar).
While intolerances can cause discomfort (like gas, bloating, and diarrhea), they are not life-threatening.
Insect Sting & Bite Allergies
For most people, an insect sting results in a temporary, painful, local reaction with redness and swelling at the site.
For those with an insect venom allergy, however, a sting can trigger a severe systemic reaction, including anaphylaxis.
The most common culprits are stinging insects from the Hymenoptera order:
- Honeybees
- Wasps
- Hornets
- Yellow jackets
- Fire ants
Biting insects like mosquitoes and fleas typically cause only local, itchy reactions and rarely trigger a systemic allergic response.
Drug Allergies
A drug allergy is an adverse reaction involving the immune system to a medication.
Any drug—prescription, over-the-counter, or herbal—can cause an allergy, but some are more common offenders:
- Penicillin and related antibiotics
- Sulfa drugs
- Aspirin, ibuprofen, and other nonsteroidal anti-inflammatory drugs (NSAIDs)
- Anticonvulsants
- Chemotherapy drugs
- Anesthetics
Symptoms can range from a mild skin rash to severe anaphylaxis.
It’s vital to differentiate a true drug allergy from a drug’s known side effects (e.g., nausea from an antibiotic).
Always inform all healthcare providers of any known or suspected drug allergies.
Skin & Contact Allergies
These allergies result from direct contact with an allergen, leading to a reaction known as allergic contact dermatitis.
The reaction is often delayed, appearing 24 to 72 hours after exposure. Common triggers include:
- Metals: Nickel, a common component in jewelry, buckles, and coins, is a leading cause. Cobalt and chromium are other metallic triggers.
- Latex: Found in gloves, balloons and condoms.
- Fragrances and Preservatives: Chemicals used in perfumes, cosmetics, soaps and lotions.
- Poison Ivy, Oak and Sumac: The allergic reaction is caused by an oil called urushiol found in these plants.
- Hair Dyes: Particularly those containing paraphenylenediamine (PPD).
Why Are Allergies Becoming More Common?
The significant rise in the prevalence of allergic diseases over the past 50 years, particularly in industrialized nations, is a well-documented phenomenon that has puzzled scientists.
While genetics certainly play a role—if your parents have allergies, you are more likely to have them—genes alone cannot explain this rapid increase.
Research points to a complex interplay of environmental and lifestyle factors, with the “Hygiene Hypothesis” being one of the most prominent theories.
The Hygiene Hypothesis
First proposed in the late 1980s, the Hygiene Hypothesis suggests that a lack of exposure to microbes, parasites, and infections during early childhood may suppress the natural development of the immune system.
In overly clean, sanitized environments, the immune system doesn’t get the “training” it needs to distinguish between harmless substances and real threats.
As a result, it becomes improperly regulated and more likely to mount an attack against benign allergens like pollen or food proteins.
An updated version of this theory, the “Old Friends” Hypothesis, posits that the immune system co-evolved with exposure to a wide range of microorganisms. Modern lifestyles—with smaller families, cleaner water, antibiotic use, and less contact with farm animals and soil—have deprived us of contact with these “old friends”, leading to immune dysregulation and a rise in inflammatory conditions like allergies and autoimmune diseases.
Other Contributing Factors
- Environmental Pollution: Air pollutants, such as diesel exhaust particles, can act as adjuvants, meaning they can enhance the allergic response to allergens like pollen, making symptoms more severe.
- Climate Change: Warmer temperatures and higher carbon dioxide levels are leading to longer and more intense pollen seasons. A study published in PNAS found that the U.S. pollen season is now 20 days longer and 21% more intense than it was in 1990, directly impacting those with seasonal allergies.
- Changes in Diet: The Western diet, high in processed foods and low in fiber and fresh produce, may alter the gut microbiome—the community of bacteria in our digestive system. A healthy microbiome is crucial for proper immune system development, and disruptions to it have been linked to an increased risk of food allergies.
- Vitamin D Deficiency: Some research suggests a link between lower levels of Vitamin D, which is important for immune regulation, and a higher risk of allergies. Reduced sun exposure in modern lifestyles may contribute to this.
Diagnosis and Professional Medical Guidance
How Are Allergies Diagnosed? A Guide to Allergy Tests
A proper diagnosis is the cornerstone of effective allergy management.
While your symptoms may strongly suggest an allergy, identifying the specific trigger(s) requires a systematic approach from a healthcare professional, ideally a board-certified allergist/immunologist.
The diagnostic process is more than just a single test, it’s a clinical investigation that combines your personal history with objective test results.
The Initial Consultation: Your Medical History
The most important step in diagnosing an allergy is a thorough discussion of your medical history.
Your doctor will ask detailed questions to uncover patterns and potential triggers. Be prepared to discuss:
- Your specific symptoms: What are they, how severe are they, and how long do they last?
- Timing and environment: When and where do your symptoms occur? Are they worse during certain seasons, in specific locations (indoors vs. outdoors) or around certain animals?
- Dietary history: For suspected food allergies, you may be asked to keep a detailed food diary, noting everything you eat and any subsequent reactions.
- Family history: A family history of allergies, asthma, or eczema increases your own risk.
- Response to medications: Have you tried any over-the-counter allergy medications and did they help?
This history allows the allergist to form a hypothesis about your potential triggers, which then guides the selection of the most appropriate tests.
Skin Prick Test (SPT)
The skin prick test is the most common, rapid, and cost-effective method for diagnosing allergies to airborne substances and foods.
- Process: A nurse or technician places small drops of purified liquid allergens on your skin, usually on the forearm or back. They then use a small, sterile probe to gently prick or scratch the skin through the drop, allowing a tiny amount of the allergen to enter the top layer of skin. The test is generally not painful, feeling like a light scratch.
- What it shows: If you are sensitized to an allergen, the specific IgE on your skin’s mast cells will trigger the release of histamine. This causes a localized reaction: a raised, red, itchy bump called a wheal, surrounded by a flush of redness called a flare. This reaction typically appears within 15-20 minutes.
- Best for: Identifying allergies to pollen, mold, pet dander, dust mites and most foods.
Blood Test (Specific IgE Test)
A blood test, also known as a specific IgE (sIgE) or RAST test, is another way to measure for sensitization to allergens.
- Process: A single blood sample is drawn and sent to a laboratory. The lab analyzes the blood for the presence and amount of specific IgE antibodies to dozens of different allergens.
- When it’s used: A blood test is a valuable alternative when a skin test cannot be performed. This may be because the patient:
- Has a severe skin condition like eczema or psoriasis that would interfere with reading the results.
- Is taking a medication that cannot be stopped (like an antihistamine) that would block the skin test reaction.
- Is highly sensitive and at risk of a severe reaction even from the tiny amount of allergen used in a skin test.
- What it shows: The test provides a numerical value for the level of IgE antibodies to a specific allergen. However, a positive result indicates sensitization, not necessarily a clinical allergy. The results must be interpreted by the allergist in the context of the patient’s medical history.
Patch Test
The patch test is the gold standard for diagnosing a different type of allergic reaction: delayed-type hypersensitivity, specifically allergic contact dermatitis.
- Process: Small amounts of suspected allergens (like nickel, latex or fragrance chemicals) are applied to patches. These patches are then placed on the patient’s back. The patches remain in place for 48 hours, during which time the patient must keep the area dry. After 48 hours, the patient returns to the office to have the patches removed. The skin is examined for any reaction, and there is often a final reading at 72 or 96 hours.
- What it shows: A positive result is a localized rash, which may include redness, swelling, or blistering at the site where the trigger allergen was applied.
- Best for: Diagnosing allergies to metals, fragrances, preservatives, hair dyes, and other chemicals that cause skin rashes upon contact.
Oral Food Challenge (OFC)
The oral food challenge is considered the most definitive and accurate test for confirming or ruling out a food allergy.
- Process: This test must only be performed under the strict supervision of an allergist in a clinical setting equipped to handle a severe reaction. The patient is given a small, gradually increasing amount of the suspected food allergen over several hours. They are monitored closely for any signs of a reaction. If no symptoms occur after consuming a full, age-appropriate serving, the allergy is ruled out.
- Gold Standard: The OFC is used when the medical history and other test results (skin or blood tests) are inconclusive. It can help confirm a diagnosis, determine if a child has outgrown a food allergy, or prove that a food is safe to eat, thereby expanding the patient’s diet.
Key Point on Testing
It’s critical to understand that a positive skin or blood test indicates sensitization, not necessarily a clinical allergy. Some people may have IgE antibodies to a substance but can eat or be exposed to it without any reaction. An allergist must correlate test results with your specific history of symptoms to make an accurate diagnosis.
Comparison of Allergy Tests
| Test Type | Procedure | Best For | Time to Result |
|---|---|---|---|
| Skin Prick Test (SPT) | Allergen extract is pricked into the skin’s surface. | Airborne allergens (pollen, dander), food allergies, penicillin. | 15-20 minutes |
| Blood Test (Specific IgE) | A blood sample is sent to a lab to measure IgE antibodies. | Patients who can’t have skin tests, confirms sensitization. | Several days to a week |
| Patch Test | Allergen patches are applied to the back for 48 hours. | Delayed skin reactions (contact dermatitis) from chemicals, metals, etc. | 48-96 hours |
| Oral Food Challenge (OFC) | Patient eats gradually increasing amounts of a food under medical supervision. | Definitively confirming or ruling out a food allergy. | 4-6 hours (in-office) |
When Should You See a Doctor for Your Allergies?
While mild seasonal allergies can often be managed with over-the-counter products, there are clear signs that it’s time to seek professional medical advice.
Consulting a doctor or allergist can lead to a more accurate diagnosis, a more effective treatment plan and a significant improvement in your quality of life.
Consider making an appointment if you experience any of the following:
- Ineffective OTC Medications: If over-the-counter antihistamines, decongestants, or nasal sprays do not provide adequate relief, or if they cause bothersome side effects like drowsiness.
- Interference with Daily Life: When your allergy symptoms are severe enough to disrupt your sleep, affect your performance at work or school, or prevent you from enjoying your usual activities.
- Chronic Sinus Infections, Headaches or Nasal Congestion: Persistent symptoms can indicate that underlying allergies are not well-controlled and are leading to complications.
- Co-existing Asthma: Allergies and asthma are closely linked. Uncontrolled allergies are a common trigger for asthma attacks. An allergist can develop a unified treatment plan to manage both conditions. According to the Asthma and Allergy Foundation of America (AAFA), managing allergic triggers is a key component of asthma control.
- Suspected Food or Drug Allergy: If you have had any reaction—even a mild one like hives or an upset stomach—after eating a specific food or taking a medication, it is crucial to be evaluated.
- CRUCIAL RED FLAG: If you have ever experienced symptoms of a severe reaction (anaphylaxis), such as difficulty breathing, swelling of the lips or throat, or dizziness after exposure to a potential allergen. You need to see an allergist immediately to confirm the trigger, obtain a prescription for an epinephrine auto-injector, and receive an emergency action plan.
A Comprehensive Guide to Allergy Treatment and Management
Managing allergies is a multi-faceted approach that goes far beyond simply popping a pill when symptoms strike.
The most effective strategies involve a layered plan tailored to your specific triggers, symptoms and lifestyle.
The goal is not just to treat reactions but to prevent them from occurring in the first place.
The modern allergy management pyramid is built on a foundation of avoidance, supported by medications, and in some cases, topped by therapies that can modify the disease itself.
What Are the Best Treatments for Allergies?
Treatment options for allergies are more advanced and varied than ever before.
They range from simple environmental controls to sophisticated biologic drugs.
An allergist can help you navigate these options to find the combination that works best for you.
Allergen Avoidance (The First Line of Defense)
The most logical and effective step in managing allergies is to avoid the triggers that cause them.
While not always easy, reducing your exposure can significantly decrease your need for medication and improve your symptoms.
- For Pollen Allergies: Monitor local pollen counts (available online or via weather apps). On high-pollen days, keep windows and doors closed, use air conditioning, and limit outdoor activities, especially in the morning when counts are highest. Shower and change clothes after coming inside to wash off pollen.
- For Dust Mite Allergies: Encase pillows, mattresses, and box springs in allergen-proof zippered covers. Wash all bedding weekly in hot water (at least 130°F / 54°C). Use a vacuum with a HEPA filter and aim to reduce indoor humidity below 50%.
- For Pet Allergies: The most effective solution is to remove the pet from the home, though this is often emotionally difficult. If that’s not an option, keep pets out of the bedroom at all times, use a HEPA air purifier, and wash your hands immediately after petting an animal.
- For Food Allergies: This requires constant vigilance. Learn to read food labels meticulously, as allergens can be hidden in unexpected ingredients. When dining out, clearly communicate your allergy to the restaurant staff. Be aware of cross-contamination risks in kitchens.
Over-the-Counter (OTC) Medications
A wide array of effective medications are available without a prescription and form the mainstay of treatment for many people.
- Antihistamines: These drugs work by blocking the action of histamine, the chemical responsible for many allergy symptoms.
- Second-generation (non-drowsy): Cetirizine (Zyrtec), Loratadine (Claritin), and Fexofenadine (Allegra) are preferred for daytime use as they cause minimal drowsiness.
- First-generation (drowsy): Diphenhydramine (Benadryl) is effective but can cause significant sedation and is generally recommended for short-term or nighttime use.
- Nasal Corticosteroids: These nasal sprays are considered the single most effective treatment for allergic rhinitis. They work by reducing inflammation in the nasal passages. Examples include Fluticasone (Flonase), Budesonide (Rhinocort), and Triamcinolone (Nasacort). They are most effective when used daily throughout the allergy season.
- Decongestants: Available as pills (Pseudoephedrine, Phenylephrine) or nasal sprays (Oxymetazoline), these drugs shrink swollen nasal tissues to relieve congestion. However, they should be used with caution. Oral decongestants can raise blood pressure, and nasal decongestant sprays, if used for more than three days, can cause severe rebound congestion.
- Mast Cell Stabilizers: Cromolyn sodium is available as a nasal spray and is very safe, but it is less effective than nasal steroids and must be used multiple times a day to prevent symptoms.
Prescription Medications
When OTC options are insufficient, your doctor may prescribe stronger or different types of medication.
- Leukotriene Modifiers: Montelukast (Singulair) is a pill that blocks the action of leukotrienes, another set of inflammatory chemicals released during an allergic reaction. It can be particularly helpful for patients who also have asthma.
- Prescription Antihistamine and Steroid Nasal Sprays: Sprays like Azelastine (an antihistamine) or combination sprays like Dymista (Azelastine and Fluticasone) can provide more potent relief than single-agent OTC products.
- Ipratropium Bromide Nasal Spray: This medication can be effective specifically for treating a severely runny nose by drying up nasal secretions.
Immunotherapy (Altering the Allergic Response)
For those with severe or persistent allergies, immunotherapy is the only treatment that can alter the natural course of the disease, making the body less allergic over time.
- Allergy Shots (Subcutaneous Immunotherapy – SCIT): This is the traditional and most well-studied form of immunotherapy. It involves receiving regular injections of gradually increasing doses of your specific allergens. Over time (typically 3-5 years), this process helps your immune system build tolerance, reducing or even eliminating your symptoms. It is highly effective for allergies to pollen, dust mites, pet dander and insect stings.
- Sublingual Immunotherapy (SLIT): A needle-free alternative, SLIT involves placing a tablet or liquid drops containing allergen extracts under your tongue daily. The FDA has approved SLIT tablets for allergies to specific grasses, ragweed, and dust mites. It is a convenient option that can be taken at home after the first dose in the doctor’s office.
Emergency Epinephrine
For anaphylaxis, epinephrine is the only life-saving treatment.
Individuals with a history of severe reactions, particularly to foods or insect stings, must carry an epinephrine auto-injector (e.g., EpiPen, Auvi-Q, Adrenaclick) at all times.
- Action: Epinephrine works rapidly to reverse the most dangerous symptoms of anaphylaxis. It constricts blood vessels to increase blood pressure, relaxes airway muscles to improve breathing, and reduces swelling and hives.
- Usage: It must be administered immediately at the first sign of a severe reaction. After using the auto-injector, it is imperative to call 911 and go to the nearest emergency room, as a second, delayed (biphasic) reaction can occur hours later.
How Can I Allergy-Proof My Home Environment?
Creating a low-allergen sanctuary at home is a proactive strategy that can dramatically reduce your daily symptom burden. Focus your efforts on the bedroom, where you spend a third of your life.
Room-by-Room Strategies:
In the Bedroom:
- Use allergen-proof covers on your mattress, box spring, and pillows. These create a barrier between you and dust mites.
- Wash sheets, blankets, and pillowcases weekly in water that is at least 130°F (54.4°C) to kill dust mites.
- Remove wall-to-wall carpeting if possible. Hardwood, tile, or linoleum floors are much easier to keep free of allergens. If you have carpet, vacuum weekly with a HEPA-filter vacuum.
- Keep pets out of the bedroom. This single step can significantly reduce your exposure to pet dander overnight.
Throughout the House:
- Control Humidity: Keep indoor humidity below 50% using a dehumidifier or air conditioner. Dust mites and mold thrive in humid environments.
- Improve Air Filtration: Use high-efficiency filters (MERV 11 or 12) in your central heating and air conditioning system and change them every 1-3 months. Consider using a portable HEPA air purifier in the bedroom or main living area.
- Clean Smart: Dust with a damp cloth instead of a dry one to trap allergens instead of sending them airborne. Wear a mask while cleaning to avoid inhaling dust and mold.
- Prevent Mold Growth: Use exhaust fans in bathrooms and the kitchen to vent moisture. Fix any leaks promptly. Clean any visible mold with a solution of detergent and water, or a 5% bleach solution for non-porous surfaces.
Part 5: Frequently Asked Questions and Conclusion
Frequently Asked Questions (FAQ) About Allergies
1. Can you develop allergies as an adult?
Yes. While many allergies begin in childhood, it is common to develop new allergies at any point in adulthood. This can happen due to changes in your environment (like moving to a new region with different pollens) or other unknown factors that shift your immune response.
2. Can allergies go away on their own?
Sometimes. Childhood allergies, particularly to milk and eggs, are often outgrown. However, allergies to peanuts, tree nuts, and seafood tend to be lifelong. Seasonal allergies can also fluctuate in severity over a person’s life but rarely disappear completely without treatment like immunotherapy.
3. What is the difference between an allergy and a cold?
Allergies are caused by an immune overreaction and often feature intense itching (eyes, nose) and clear, watery mucus. Colds are caused by viruses and are more likely to involve a sore throat, body aches, and thicker, colored mucus. Colds typically last 7-10 days, while allergies persist as long as you’re exposed to the allergen.
4. Are “hypoallergenic” pets truly safe for people with allergies?
No. There is no such thing as a truly hypoallergenic cat or dog. The allergens are proteins found in the animal’s dander, saliva, and urine, not their fur. While some breeds may shed less, all animals produce the allergen. The only way to know if you’ll react is to spend time with the specific animal.
5. Does eating local honey help with pollen allergies?
This is a popular myth, but there is no scientific evidence to support it. The theory is that it acts like a form of immunotherapy. However, the pollen in honey is from flowers, which is carried by bees, not the light, airborne pollen from trees, grasses and weeds that causes most seasonal allergies.
6. What is Oral Allergy Syndrome (OAS)?
OAS, or Pollen-Food Allergy Syndrome, occurs in people with pollen allergies. Certain raw fruits, vegetables, and nuts contain proteins that are structurally similar to pollen proteins. This cross-reactivity can cause an itchy mouth, throat, or mild swelling when these foods are eaten. Cooking the food usually breaks down the protein and prevents a reaction.
7. Can stress make my allergies worse?
Yes. Stress hormones, like cortisol, can have a complex effect on the immune system. Chronic stress can dysregulate immune responses and increase inflammation, potentially making your body more reactive to allergens and your symptoms feel more severe.
8. Is it possible to be allergic to water or sunlight?
Not in the true IgE-mediated sense. However, there are rare conditions that mimic allergies. Aquagenic urticaria is a condition where contact with water causes hives, but it’s not a true allergy. Solar urticaria is a similar condition where sun exposure triggers hives, likely due to a reaction to a light-altered substance in the skin.
Conclusion
Allergies, in their many forms, represent a fundamental miscommunication within the body’s defense system.
While they can range from a seasonal annoyance to a constant, life-altering threat, they are a manageable medical condition.
The journey to effective control begins with knowledge—understanding that an itchy nose, a skin rash, or digestive distress is the end result of a complex immune cascade involving IgE, mast cells and histamine.
The key takeaways from this guide are clear: accurate diagnosis is the essential first step.
Pinpointing your specific triggers through a combination of medical history and validated testing with an allergist provides the roadmap for your management plan.
This plan is a dynamic, personalized strategy built on three pillars: intelligent avoidance of your triggers, judicious use of effective medications to control symptoms, and for many, the disease-modifying potential of immunotherapy to build long-term tolerance.
Living with allergies does not have to mean living with limitations. By understanding the science behind your condition and partnering with a healthcare professional, you are empowered to make informed decisions.
You can transform your home into a low-allergen environment, navigate the world with confidence, and choose the right treatments to reclaim your comfort and quality of life. Your allergies are a part of you, but they do not have to define you.
If you are struggling with symptoms you believe are caused by allergies, we strongly encourage you to consult with a healthcare professional or a board-certified allergist.
They can provide a personalized diagnosis and a comprehensive management plan to help you live a fuller, more comfortable life.
We invite you to share your own experiences with allergies or ask any further questions in the comments section below. Your story could help others on their own journey.

