You can naturally reduce chronic inflammation through targeted, science-backed lifestyle changes.
The most effective methods include adopting an anti-inflammatory diet rich in whole foods, managing stress, ensuring quality sleep, and engaging in regular, moderate exercise.
These strategies work together to calm your body’s overactive immune response.
While a little inflammation is good—it’s your body’s first line of defense against injury and infection—a persistent, low-grade version of this process can become a silent threat.
This is known as chronic inflammation. According to the Centers for Disease Control and Prevention (CDC), a staggering 6 in 10 adults in the US have a chronic disease, and 4 in 10 have two or more.
Many of these conditions, including heart disease, type 2 diabetes, and arthritis, are fundamentally linked to this underlying, unresolved inflammation.
This guide is designed to be your definitive resource for understanding and combating chronic inflammation.
We will demystify the science, distinguishing between beneficial acute inflammation and harmful chronic inflammation.
You will discover 10 actionable, evidence-based strategies—from the foods you eat to the way you sleep—that can profoundly lower inflammation levels in your body.
By the end of this article, you will have a practical, holistic plan to reclaim your health and vitality. Read on to take the first step.
In This Article
Foundational Knowledge: Understanding Inflammation
Before we dive into the solutions, it’s crucial to understand the problem.
The term “inflammation” is often used with negative connotations, but the reality is more nuanced.
Understanding the difference between the body’s necessary, protective response and a dysfunctional, chronic state is the first step toward effective management.
What Exactly Is Inflammation?
At its core, inflammation is a vital part of the immune system’s response to harmful stimuli, such as pathogens, damaged cells, or irritants.
Think of it as your body’s biological first-responder team.
Its primary purpose is to eliminate the initial cause of cell injury, clear out dead cells and tissues and initiate tissue repair.
This process is most recognizable in its acute form.
Imagine you get a small cut on your finger. Within moments, your immune system dispatches an army of white blood cells to the site.
This response produces the classic signs of acute inflammation:
- Redness (Rubor): Caused by increased blood flow to the area.
- Heat (Calor): Also a result of increased blood flow.
- Swelling (Tumor): From the accumulation of fluid.
- Pain (Dolor): Due to the release of chemicals that stimulate nerve endings.
As Harvard Health Publishing explains, this type of inflammation is not only normal but essential for healing.
It’s a short-term, robust, and self-limiting process.
Once the threat is neutralized and the healing is underway, the inflammatory response subsides.
“Some inflammation is good. Too much is often bad. The goal is to recognize when inflammation is simply doing its job, and when it can potentially cause problems”. – Dr. Robert H. Shmerling, Harvard Medical School
The problem arises when this response doesn’t turn off.
This leads to chronic inflammation, a slow, long-term inflammatory state that can last for months or even years.
It’s like a fire alarm that continues to blare long after the fire has been extinguished, eventually causing its own damage.
In this state, the immune system persistently releases inflammatory cells and substances, which can eventually damage healthy tissues, cells and organs.
Why Is Chronic Inflammation a Major Health Concern?
Chronic inflammation is often described as a “silent killer” because it can develop without obvious symptoms, slowly undermining your health from the inside.
Unlike acute inflammation, it doesn’t always produce noticeable pain or redness. Instead, its effects are systemic and cumulative.
A growing body of research has firmly linked chronic inflammation to the development and progression of most of the deadliest and most debilitating diseases of our time. These include:
- Cardiovascular Disease: Inflammation plays a key role in atherosclerosis, the process where plaque builds up in arteries, leading to heart attacks and strokes.
- Type 2 Diabetes: Chronic inflammation can contribute to insulin resistance, a hallmark of type 2 diabetes.
- Cancer: A chronic inflammatory environment can promote tumor growth, proliferation and metastasis.
- Neurodegenerative Diseases: Conditions like Alzheimer’s and Parkinson’s disease have a significant inflammatory component.
- Autoimmune Disorders: In conditions like rheumatoid arthritis and lupus, the immune system mistakenly attacks the body’s own tissues, driven by inflammation.
- Chronic Kidney Disease, Fatty Liver Disease, and more.
A 2024 study published in *Pharmacological Research* highlights the urgent need for interventions targeting systemic inflammation to prevent cardiovascular diseases, underscoring its role as a central pathological mechanism.
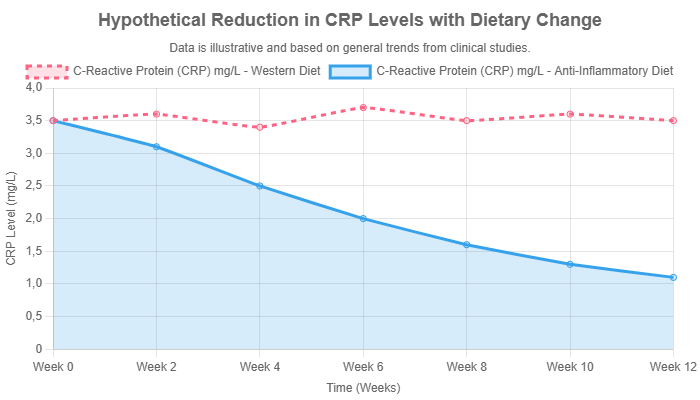
So, how do doctors detect this invisible threat? One of the most common methods is a blood test for inflammatory biomarkers.
The most widely used marker is C-reactive protein (CRP), a substance produced by the liver in response to inflammation.
A high-sensitivity CRP (hs-CRP) test can detect low but persistent levels of inflammation.
According to numerous studies, an hs-CRP level between 1 and 3 mg/L can signal a low-grade, chronic inflammatory state that increases cardiovascular risk .
This test provides a tangible way to measure the body’s inflammatory burden and track the effectiveness of lifestyle interventions.
The Core Strategy: 10 Proven Natural Ways to Reduce Inflammation
Combating chronic inflammation doesn’t necessarily require a pharmacy.
Your daily choices have a profound impact on your body’s inflammatory state.
Here, we explore ten powerful, natural strategies grounded in scientific evidence that can help you reduce inflammation and build a foundation for long-term health.
1. How Can an Anti-Inflammatory Diet Protect Your Body?
The single most powerful tool you have to control inflammation is your diet.
The foods you eat can either promote or quell the inflammatory fire.
An anti-inflammatory diet isn’t a restrictive, short-term plan, it’s a sustainable pattern of eating that emphasizes whole, nutrient-dense foods.
The Principles of Anti-Inflammatory Eating
The core principle is simple: eat more foods that fight inflammation and fewer foods that cause it.
This means focusing on foods rich in antioxidants and polyphenols.
These compounds help neutralize unstable molecules called free radicals, which can cause cellular damage and trigger an inflammatory response.
The Mediterranean diet is often cited as a gold-standard example of an anti-inflammatory eating pattern, linked to reduced inflammatory markers and lower risk of chronic disease.
Powerhouse Foods to Embrace
- Leafy Greens & Vegetables: Spinach, kale, broccoli, and cauliflower are packed with antioxidants and vitamins like Vitamin K, which has anti-inflammatory properties. Their high fiber content also supports a healthy gut microbiome, which is crucial for regulating inflammation.
- Fatty Fish: Salmon, mackerel, sardines, and herring are rich in the omega-3 fatty acids EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid). These fats are converted in the body into powerful anti-inflammatory compounds called resolvins and protectins, which actively help resolve inflammation.
- Berries & Cherries: Blueberries, strawberries, raspberries and tart cherries are loaded with antioxidants called anthocyanins. Studies have shown that these compounds can significantly lower inflammatory markers.
- Nuts & Seeds: Almonds, walnuts, and chia seeds provide a combination of healthy monounsaturated and polyunsaturated fats, fiber and antioxidants. Walnuts are particularly high in the plant-based omega-3 ALA.
- Healthy Fats: Extra virgin olive oil is a cornerstone of the Mediterranean diet. Its main antioxidant, oleocanthal, has been shown to have anti-inflammatory effects similar to ibuprofen. Avocados are another excellent source of healthy monounsaturated fats and antioxidants.
2. What Spices Are Best for Fighting Inflammation?
Your spice rack can be a powerful arsenal in the fight against inflammation.
Certain spices contain highly concentrated bioactive compounds that have been studied for their potent medicinal properties.
Turmeric (Curcumin): The Golden Spice
Turmeric, the bright yellow spice used in curry, contains a powerful compound called curcumin.
Curcumin is a polyphenol that has been extensively studied for its anti-inflammatory effects.
It works by blocking NF-κB, a molecule that travels into the nuclei of your cells and turns on genes related to inflammation.
Its potency is considered comparable to some anti-inflammatory drugs, but without the side effects.
Pro Tip: Curcumin is poorly absorbed on its own. To enhance its bioavailability, always consume it with black pepper, which contains piperine, a natural substance that can increase curcumin absorption by up to 2.000%. Adding a source of healthy fat, like olive oil, also aids absorption.
Ginger: A Potent Anti-Inflammatory Root
Ginger has been used for centuries in traditional medicine to treat a wide range of ailments. Its anti-inflammatory properties come from its main bioactive compounds, gingerols and shogaols.
These substances can inhibit the production of pro-inflammatory cytokines.
Clinical trials have shown that ginger can be effective in reducing pain and inflammation associated with osteoarthritis.
3. Does Exercise Really Help Reduce Inflammation?
Yes, absolutely. Regular physical activity is a cornerstone of an anti-inflammatory lifestyle.
While intense, exhaustive exercise can temporarily increase inflammation, consistent, moderate-intensity exercise has a powerful systemic anti-inflammatory effect.
The mechanism is fascinating. A landmark 2017 study published in Brain, Behavior, and Immunity found that just 20 minutes of moderate exercise, such as brisk walking on a treadmill, was enough to stimulate the nervous system to produce an anti-inflammatory cellular response.
Exercise triggers the release of adrenaline and noradrenaline, which in turn suppress the production of TNF, a key pro-inflammatory cytokine.
The key is consistency. Aim for at least 150 minutes of moderate-intensity aerobic exercise (like brisk walking, swimming or cycling) or 75 minutes of vigorous-intensity exercise per week, as recommended by health authorities.
This not only directly reduces inflammation but also helps manage weight, improve insulin sensitivity and reduce stress—all of which contribute to a lower inflammatory state.
4. How Does Sleep Quality Affect Inflammation Levels?
Sleep is not a passive state, it’s a critical period of restoration and regulation for the entire body, including the immune system.
A lack of quality sleep is a significant physiological stressor that can throw your inflammatory response into overdrive.
Research has consistently shown that sleep deprivation, or even just poor-quality sleep, leads to elevated levels of inflammatory markers like C-reactive protein (CRP) and interleukin-6 (IL-6).
During sleep, the body performs essential housekeeping tasks, including regulating cytokine production.
When sleep is disrupted, this regulation falters, leading to a pro-inflammatory state.
To improve your sleep hygiene and lower inflammation:
- Maintain a Consistent Schedule: Go to bed and wake up around the same time every day, even on weekends.
- Create a Dark, Cool, Quiet Environment: Use blackout curtains, keep the temperature cool and minimize noise.
- Avoid Blue Light Before Bed: Stop using screens (phones, tablets, TVs) at least an hour before sleep, as the blue light can suppress melatonin production.
- Limit Caffeine and Alcohol: Avoid caffeine in the afternoon and evening. While alcohol may make you feel sleepy initially, it disrupts sleep architecture later in the night.
5. What Is the Link Between Stress and Inflammation?
The connection between your mind and your immune system is powerful.
While short-term stress can be adaptive, chronic psychological stress is a major driver of chronic inflammation.
When you’re stressed, your adrenal glands release the hormone cortisol.
In the short term, cortisol is actually anti-inflammatory.
However, under conditions of chronic stress, your body’s cells can become resistant to cortisol’s regulatory effects.
This cortisol resistance allows inflammation to run rampant, as the “brakes” on the immune response are no longer effective.
This process is linked to a host of stress-related diseases.
Implementing stress-management techniques is therefore a non-negotiable part of an anti-inflammatory lifestyle. Evidence-based methods include:
- Mindfulness and Meditation: Practices that train you to focus on the present moment can lower stress and have been shown to reduce inflammatory markers.
- Yoga and Tai Chi: These mind-body practices combine physical postures, breathing exercises, and meditation to reduce stress and improve physical function.
- Spending Time in Nature: Often called “forest bathing”, spending time in natural environments has been shown to lower cortisol levels and reduce inflammation.
6. Why Should You Limit Sugar and Refined Carbs?
While some foods fight inflammation, others actively promote it.
At the top of the list of “foods that cause inflammation” are added sugars and refined carbohydrates.
When you consume high amounts of sugar (especially high-fructose corn syrup) and refined carbs (like white bread, pastries, and white pasta), your blood sugar spikes.
This can lead to an increase in pro-inflammatory messengers.
Furthermore, excess sugar in the bloodstream can attach to proteins and fats in a process called glycation, forming harmful compounds called Advanced Glycation End Products (AGEs).
AGEs are highly inflammatory and can cause oxidative stress, damaging cells and contributing to aging and disease.
Reducing your intake of sugary drinks, desserts, processed snacks, and refined grains is one of the most direct ways to lower your body’s inflammatory burden.
7. Can Omega-3 Fatty Acids Lower Inflammation?
Yes, and their role is so critical it deserves its own section.
The balance between omega-6 and omega-3 fatty acids in your diet is a key regulator of inflammation.
While both are essential, the typical Western diet contains far too many omega-6s (found in processed seed and vegetable oils like soy and corn oil) and not enough omega-3s.
Omega-6s are precursors to pro-inflammatory molecules, while omega-3s are precursors to anti-inflammatory molecules.
An imbalanced ratio promotes a chronic inflammatory state. To shift the balance:
- Increase Omega-3s: As mentioned, fatty fish are the best source of EPA and DHA. Plant-based sources like flaxseeds, chia seeds, and walnuts provide ALA, which the body can convert to EPA and DHA, though inefficiently.
- Decrease Omega-6s: Reduce your consumption of processed foods and vegetable oils high in omega-6s. Cook with olive oil or avocado oil instead.
For individuals who don’t eat fish regularly, a high-quality fish oil or algae-based omega-3 supplement may be beneficial.
However, it’s crucial to consult with a healthcare provider to determine the right dosage and ensure the product is free from contaminants.
8. How Does Hydration Impact Your Body’s Inflammatory Response?
Proper hydration is a simple yet often overlooked component of managing inflammation.
Your body relies on water for nearly every physiological process, including flushing out toxins and waste products that can contribute to inflammation.
When you are dehydrated, the concentration of inflammatory markers in your blood can increase.
Dehydration also puts stress on your kidneys, hindering their ability to filter waste.
Furthermore, it can impair the function of cartilage in your joints, which is primarily composed of water, potentially exacerbating joint pain and inflammation.
Aim to drink plenty of water throughout the day.
A good rule of thumb is to drink half your body weight in ounces.
In addition to water, unsweetened herbal teas can contribute to your fluid intake.
Green tea is an especially good choice, as it contains a powerful polyphenol called epigallocatechin-3-gallate (EGCG), which has potent anti-inflammatory and antioxidant effects.
9. Could Intermittent Fasting Help Control Inflammation?
Intermittent fasting (IF), an eating pattern that cycles between periods of eating and voluntary fasting, is an emerging area of research for inflammation control.
While more studies are needed, the initial findings are promising.
Research from the University of Cambridge (2024) has begun to uncover the mechanisms.
Fasting appears to increase a metabolite called arachidonic acid, which in turn inhibits the NLRP3 inflammasome, a key driver of inflammation.
Other studies suggest that IF can trigger autophagy, the body’s cellular cleanup process, which removes damaged cells that could otherwise trigger an inflammatory response.
IF is not suitable for everyone, particularly pregnant women, individuals with a history of eating disorders or those with certain medical conditions.
It should be considered an advanced strategy and undertaken only after consulting with a healthcare professional.
10. What Effect Does Alcohol Have on Inflammation?
The relationship between alcohol and inflammation is complex and dose-dependent.
Excessive alcohol consumption is unequivocally pro-inflammatory.
It can damage the gut lining, leading to “leaky gut“, where bacterial toxins can pass into the bloodstream, triggering a strong immune response.
It also places a heavy burden on the liver, a central organ in regulating inflammation.
On the other hand, some studies have suggested that light to moderate consumption of red wine may have anti-inflammatory benefits.
This is often attributed to resveratrol, a polyphenol found in grape skins.
However, the amount of resveratrol in wine is relatively small, and the potential risks of alcohol often outweigh the benefits.
It is not recommended to start drinking alcohol for its potential health benefits. If you do drink, moderation is key.
Practical Application and Visual Aids
Knowledge is only powerful when applied.
This section provides practical tools to help you easily implement an anti-inflammatory lifestyle.
What Foods Should You Avoid to Reduce Inflammation?
To simplify your journey, here is a clear, scannable list of the primary foods and ingredients known to promote chronic inflammation.
Limiting these is just as important as adding beneficial foods.
- Sugary Beverages: Soda, sweetened fruit juices, sports drinks, and sweet tea.
- Refined Carbohydrates: White bread, white pasta, white rice and most pastries and baked goods.
- Processed Meats: Hot dogs, sausage, bacon, and deli meats, which contain AGEs and preservatives.
- Certain Vegetable and Seed Oils: Oils high in omega-6 fatty acids, such as soybean oil, corn oil, sunflower oil, and safflower oil, especially when used in processed foods.
- Trans Fats: Found in fried foods, margarine, and many processed snacks and baked goods (often listed as “partially hydrogenated oil”).
- Excessive Alcohol: As discussed, heavy drinking promotes inflammation.
Table: Anti-Inflammatory vs. Pro-Inflammatory Food Swaps
Making changes can feel overwhelming.
Use this simple table as a quick reference guide for easy, anti-inflammatory swaps in your daily diet.
| Instead of This (Pro-Inflammatory) | Choose This (Anti-Inflammatory) |
|---|---|
| Sugary Cereal | Oatmeal with Berries, Nuts, and a sprinkle of Cinnamon |
| White Bread Sandwich | Large Salad with Grilled Salmon or Chicken |
| Soda or Sweet Tea | Water, Unsweetened Green Tea or Herbal Tea |
| Processed Sausage or Hot Dog | Grilled Salmon, Chicken Breast or Lentil Patty |
| French Fries | Baked Sweet Potato Wedges with Olive Oil and Rosemary |
| Chips and Creamy Dip | Vegetable Sticks (Carrots, Bell Peppers) with Hummus or Guacamole |
| Candy Bar | A piece of Dark Chocolate (≥70% cocoa) and a handful of Almonds |
| Soybean or Corn Oil for Cooking | Extra Virgin Olive Oil or Avocado Oil |
Chart: Illustrative Impact of Diet on Inflammatory Markers
To visualize the potential impact of dietary changes, the chart below illustrates a hypothetical reduction in C-reactive protein (CRP) levels over 12 weeks when shifting from a standard Western diet to a whole-foods, anti-inflammatory diet.
While individual results vary, this demonstrates the powerful trend observed in clinical research.
Frequently Asked Questions (FAQ)
1. What is the fastest way to reduce inflammation in the body?
The fastest way is a combined approach: immediately eliminate pro-inflammatory foods like sugar and processed items while adopting an anti-inflammatory diet rich in omega-3s and antioxidants. Combining this with moderate exercise and quality sleep can yield noticeable improvements within days to weeks.
2. What is the single best drink for inflammation?
While water is essential, green tea is arguably the single best beverage. It’s hydrating and packed with EGCG, a powerful antioxidant polyphenol with proven anti-inflammatory properties that can help reduce systemic inflammation and oxidative stress in the body.
3. Can vitamins or supplements reduce inflammation?
Yes, certain supplements like high-quality fish oil (omega-3s), curcumin (from turmeric), and Vitamin D have strong evidence for reducing inflammation. However, you should always consult a healthcare professional before starting any new supplement regimen to ensure safety and proper dosage.
4. How long does it take to reduce inflammation through diet?
While some people report feeling better within a week, significant changes in inflammatory biomarkers like CRP can typically be measured within 4 to 12 weeks of consistent dietary changes. The long-term benefits continue to build over time.
5. Does drinking coffee increase or decrease inflammation?
For most people, coffee appears to be anti-inflammatory. It is rich in polyphenols and other antioxidant compounds that have been linked to lower levels of inflammatory markers. However, individual reactions can vary, especially if loaded with sugar and cream.
6. Is cheese inflammatory?
It’s complicated. Cheese is high in saturated fat, which can be pro-inflammatory for some. However, fermented dairy like yogurt and some cheeses also contain probiotics, which can be anti-inflammatory. It’s best consumed in moderation as part of a balanced diet.
7. Can losing weight reduce inflammation?
Yes, significantly. Adipose (fat) tissue, particularly visceral fat around the organs, is metabolically active and produces pro-inflammatory cytokines. Losing excess weight is one of the most effective ways to lower your body’s overall inflammatory load.
8. What are the first signs of chronic inflammation?
The signs are often subtle and non-specific. They can include persistent fatigue, body aches or joint pain, digestive issues like constipation or diarrhea, skin problems like eczema or psoriasis, and frequent infections. A blood test for CRP is a more definitive measure.
Conclusion
Chronic inflammation is a formidable adversary, silently contributing to many of the most serious health challenges of our time.
However, it is not an uncontrollable force.
As we’ve explored, you hold a remarkable degree of power to manage and reduce your body’s inflammatory burden through conscious, daily choices.
The journey to lower inflammation is not about a single “superfood” or a quick-fix pill.
It is a long-term commitment to a holistic lifestyle built on four key pillars:
- A nutrient-dense, anti-inflammatory diet.
- Consistent, moderate exercise.
- Restorative, high-quality sleep.
- Effective stress management.
By embracing these strategies, you are not just fighting inflammation, you are building a foundation of resilience and vitality that will serve you for years to come.
The path forward may seem daunting, but it doesn’t require a complete overhaul overnight.
We encourage you to start small.
Pick one or two strategies from this guide—perhaps swapping your sugary soda for green tea or adding a 20-minute walk to your daily routine—and implement them this week.
Small, consistent steps are the key to lasting change.
We invite you to share your own experiences, questions, or successes in the comments section below.
Your journey can inspire others, and together, we can build a community dedicated to taking control of our health.
References
- CDC – About Chronic Diseases
- Harvard Health Publishing – Understanding acute and chronic inflammation
- Healthline – Anti-Inflammatory Diet 101: How to Reduce Inflammation Naturally
- PubMed – Targeting systemic inflammation in metabolic disorders (2024)
- New England Journal of Medicine – C-Reactive Protein and Other Markers of Inflammation
- PubMed Central – Therapeutic Roles of Curcumin
- Brown University – Foods for Fighting Inflammation
- University of Cambridge – Scientists identify how fasting may protect against inflammation (2024)

