Finding relief from a pinched nerve often involves a combination of rest, posture correction, targeted exercises, and, in some cases, medical treatment.
The sharp, radiating pain, numbness, or tingling can be debilitating, but understanding the right steps to take can significantly speed up your recovery and restore your quality of life.
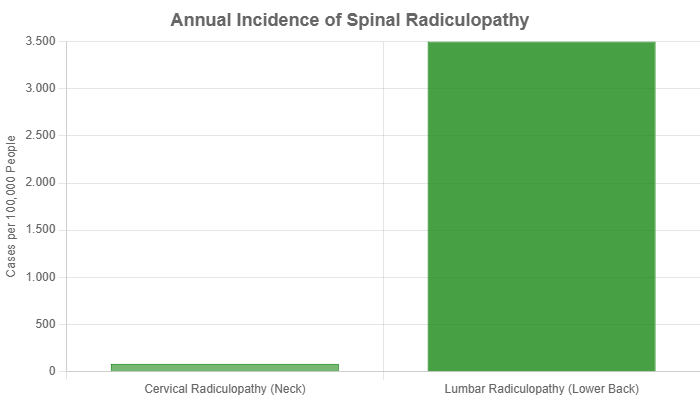
This condition is surprisingly common for instance, cervical radiculopathy (a pinched nerve in the neck) has an annual incidence of about 83 cases per 100.000 people, according to research published by the National Center for Biotechnology Information (NCBI).
This comprehensive guide will walk you through everything you need to know, from identifying the symptoms and causes to implementing evidence-based strategies for immediate and long-term relief.
In This Article
What Exactly Is a Pinched Nerve?
Before diving into treatments, it’s crucial to understand what a pinched nerve truly is.
The term itself is a common phrase, but the underlying medical condition is more complex.
Demystifying the Term: Beyond the “Pinch”
A “pinched nerve” is not a formal medical diagnosis but a lay term describing nerve compression or irritation.
Healthcare providers use more specific terms like radiculopathy, which refers to a nerve root being compressed as it exits the spine.
As the Cleveland Clinic explains, this pressure can come from surrounding tissues like bones, cartilage, muscles or tendons.
Think of a nerve as a garden hose. When something kinks or steps on the hose, the flow of water is disrupted.
Similarly, when a nerve is compressed, the flow of electrical signals is impaired, leading to pain, numbness and weakness.
Common Locations: Neck, Back and Beyond
While a pinched nerve can occur almost anywhere, the most common sites are in the spine:
- Cervical Spine (Neck): Compression here often leads to pain that radiates down the shoulder and into the arm and hand. This is known as cervical radiculopathy.
- Lumbar Spine (Lower Back): A pinched nerve in the lower back frequently affects the sciatic nerve, causing pain to travel down the buttock and leg, a condition famously known as sciatica or lumbar radiculopathy.
Other common nerve entrapment syndromes include:
- Carpal Tunnel Syndrome: Compression of the median nerve in the wrist.
- Cubital Tunnel Syndrome: Compression of the ulnar nerve at the elbow.
- Tarsal Tunnel Syndrome: Compression of the tibial nerve in the ankle.
The Science of Nerve Compression: What Happens to Your Nerves?
When a nerve is compressed, two primary things happen.
First, the physical pressure can block blood flow to the nerve (ischemia), depriving it of oxygen and nutrients.
This disruption interferes with its ability to transmit signals effectively.
Second, the compression often triggers an inflammatory response.
Tissues like a herniated disc can release chemical irritants that inflame the nerve root, making it even more sensitive and painful.
This combination of mechanical pressure and chemical irritation is what produces the classic pinched nerve symptoms.
How Do I Know If I Have a Pinched Nerve?
Distinguishing a pinched nerve from a simple muscle strain is key to getting the right treatment.
The symptoms are often distinct and follow specific patterns.
Recognizing the Telltale Symptoms
According to the Mayo Clinic, the hallmark symptoms of a pinched nerve include:
- Sharp, Aching or Burning Pain: This pain often radiates outward from the site of compression.
- Numbness or Decreased Sensation: You might notice a loss of feeling in the area supplied by the nerve.
- Tingling or “Pins and Needles” Sensation (Paresthesia): A common and unsettling feeling.
- Muscle Weakness: You may find it difficult to grip objects or notice a limb feeling “heavy”.
- A Feeling That a Hand or Foot Has “Fallen Asleep”: This sensation may be frequent or persistent.
Symptoms can often feel worse at night or with certain movements that further compress the nerve.
Symptoms Specific to Neck vs. Back
The location of your symptoms can help pinpoint where the pinched nerve is located:
- Pinched Nerve in Neck: Symptoms typically affect one side, radiating from the neck into the shoulder, arm, hand or fingers. You might experience weakness in your bicep, tricep or hand grip.
- Pinched Nerve in Back: Symptoms usually travel down the back of the leg, often past the knee and into the foot. This can cause difficulty with walking or lifting your foot (foot drop).
The Red Flags: When to See a Doctor Immediately
While most pinched nerves can be managed conservatively, some symptoms indicate a medical emergency.
Seek immediate medical attention if you experience:
- Loss of Bowel or Bladder Control: This can signal a serious condition called cauda equina syndrome.
- Progressive or Severe Weakness: If your arm or leg is becoming noticeably weaker over a short period.
- Numbness in the “Saddle” Area: Loss of sensation in the inner thighs, buttocks, and perineum.
- Symptoms Following a Significant Trauma: Such as a car accident or a fall.
What Causes a Pinched Nerve in the First Place?
Nerve compression can result from a variety of factors, ranging from gradual wear and tear to sudden injury.
Degenerative Changes: The Role of Aging
As we age, our spine naturally undergoes changes that can narrow the spaces where nerves travel.
- Herniated Discs: The soft, gel-like center of a spinal disc can push out through a tear in its tough exterior, pressing directly on a nerve root.
- Bone Spurs (Osteophytes): In response to arthritic changes, the body can grow extra bone to stabilize a joint. These bone spurs can encroach on the nerve pathways.
- Spinal Stenosis: This is a general narrowing of the spinal canal, which can put pressure on the spinal cord and/or nerve roots.
Lifestyle and Environmental Factors
Your daily habits and physical condition play a significant role:
- Repetitive Motions: Jobs or hobbies that involve repetitive movements of the wrist, shoulder or back can lead to inflammation and nerve compression.
- Poor Posture: Sustained poor posture, especially “text neck” or slouching at a desk, puts undue stress on the spine.
- Obesity: Excess body weight increases the load on the spine and can contribute to disc herniation and nerve compression.
Acute Injuries and Other Conditions
Sometimes, a pinched nerve is the result of a specific event or underlying health issue:
- Trauma: A sudden injury from a fall, sport, or accident can cause a disc to herniate or tissues to swell, compressing a nerve.
- Rheumatoid Arthritis: This autoimmune disease causes inflammation that can compress nerves in the joints.
- Pregnancy: The weight gain and fluid retention associated with pregnancy can cause swelling that leads to nerve compression, particularly carpal tunnel syndrome.
How Can I Get Immediate Relief at Home?
For most cases of a mild to moderate pinched nerve, conservative home care is the first and most effective line of defense.
The goal is to reduce inflammation and relieve pressure on the nerve.
Rest and Activity Modification
This doesn’t mean complete bed rest. The key is to stop any activities that cause or worsen your symptoms.
Avoid heavy lifting, twisting, or prolonged sitting or standing.
Gentle movement is encouraged, as it prevents stiffness and promotes blood flow.
Heat and Cold Therapy: Which One and When?
The choice between ice and heat depends on the timing of the injury.
- Cold Therapy (First 48-72 hours): Apply an ice pack wrapped in a thin towel to the affected area for 15-20 minutes at a time. This helps constrict blood vessels, reducing inflammation and numbing the pain.
- Heat Therapy (After 72 hours): Use a heating pad or warm compress to relax tight muscles that may be contributing to the nerve compression. Heat increases blood flow, which can aid the healing process.
Over-the-Counter (OTC) Pain Relievers
Nonsteroidal anti-inflammatory drugs (NSAIDs) are often recommended because they address both pain and inflammation.
As noted by Harvard Health Publishing, options like ibuprofen (Advil, Motrin) or naproxen sodium (Aleve) can be effective.
Always follow the package directions and consult a doctor if you have other health conditions.
Posture Correction and Ergonomics
Pay close attention to your posture. When sitting, ensure your feet are flat on the floor, your back is supported, and your screen is at eye level.
When standing, keep your shoulders back and your core engaged.
These small adjustments can significantly reduce pressure on your spinal nerves.
What Are the Best Exercises for a Pinched Nerve?
Once the initial, acute pain subsides, specific stretches and exercises are vital for long-term relief.
They help create space for the nerve, strengthen supporting muscles and improve flexibility.
Important: Stop any exercise that causes sharp pain. The goal is gentle stretching and strengthening, not forcing a movement.
The Foundation: Why Exercise is Crucial
Research consistently shows that a structured exercise program is a cornerstone of recovery.
A systematic review published in the Journal of Physical Therapy Science found that exercise training, incorporating both strengthening and stretching, is beneficial for improving function and reducing pain in patients with cervical radiculopathy.
Gentle Stretches for a Pinched Nerve in the Neck
- Chin Tuck: While sitting or standing tall, gently pull your chin straight back, creating a “double chin”. Hold for 5 seconds and repeat 10 times. This activates deep neck flexors and relieves pressure at the base of the skull.
- Head Tilt: Gently tilt your ear toward your shoulder until you feel a light stretch on the opposite side of your neck. Hold for 20-30 seconds. Repeat on the other side.
- Trap Stretch: Place one hand on the top of your head and gently pull your head towards your shoulder while looking slightly down. You should feel a stretch in your upper trapezius muscle. Hold for 20-30 seconds and switch sides.
Strengthening Exercises for Neck Support
Once stretching is comfortable, add gentle strengthening.
Place your palm on your forehead and press gently, resisting the motion with your neck muscles without actually moving your head (isometric contraction).
Hold for 5-10 seconds. Repeat this on the back and sides of your head.
Safe Stretches for a Pinched Nerve in the Lower Back
- Knee-to-Chest Stretch: Lie on your back with your knees bent. Gently pull one knee toward your chest until you feel a stretch in your lower back and buttock. Hold for 30 seconds and switch legs.
- Pelvic Tilt: Lie on your back with knees bent. Gently flatten your lower back against the floor by tightening your abdominal muscles. Hold for 10 seconds and repeat 10 times.
- Cat-Cow Stretch: Start on your hands and knees. Inhale as you drop your belly and look up (Cow). Exhale as you round your spine and tuck your chin (Cat). This gently mobilizes the spine.
Core Strengthening for a Stable Spine
A strong core acts as a natural brace for your spine.
Exercises like planks, bird-dog, and bridges are excellent for building core stability without putting excessive strain on your back.
When Should I Consider Professional Medical Treatment?
If home care and exercises don’t provide sufficient relief after a few weeks, or if your symptoms are severe, it’s time to seek professional help.
The Role of Physical Therapy: A Guided Recovery
A physical therapist can create a personalized treatment plan. This often includes a combination of manual therapy and therapeutic exercise.
A systematic review in the Journal of Orthopaedic & Sports Physical Therapy concluded that combining manual therapy with exercise is effective for increasing function and decreasing pain in patients with cervical radiculopathy.
Techniques may include:
- Manual Therapy: Hands-on techniques to mobilize joints and soft tissues.
- Nerve Gliding: Specific movements designed to help the nerve move more freely.
- Traction: Gentle pulling on the head or pelvis to open up the nerve pathways.
Prescription Medications: Beyond OTC Options
If OTC medications aren’t enough, your doctor might prescribe:
- Oral Corticosteroids: A short course can powerfully reduce inflammation.
- Muscle Relaxants: To alleviate painful muscle spasms that can accompany a pinched nerve.
- Neuropathic Pain Agents: Drugs like gabapentin or pregabalin can be effective for nerve-related pain.
Corticosteroid Injections: Targeted Relief
An epidural steroid injection delivers a potent anti-inflammatory medication directly to the source of the problem.
This can provide significant, albeit often temporary, pain relief, creating a window of opportunity to engage more effectively in physical therapy.
What Are the Advanced and Surgical Options?
Surgery is typically a last resort, reserved for cases with severe, persistent pain, progressive neurological deficits or when conservative treatments have failed.
Understanding Spinal Decompression Therapy
Nonsurgical spinal decompression is a motorized form of traction that aims to relieve pressure on spinal discs and nerves.
A 2022 study published in Healthcare (Basel) found that it significantly reduced the size of herniated discs on MRI and improved function in patients with lumbar radiculopathy.
While promising, it’s important to discuss with your doctor if you are a good candidate.
When is Surgery Necessary?
Surgery is generally considered if you have:
- Failed at least 6-12 weeks of structured conservative care.
- Intolerable pain that is not responding to any other treatment.
- Progressive muscle weakness or numbness.
- Signs of spinal cord compression (myelopathy).
Common Surgical Procedures Explained
- Discectomy: The surgeon removes the portion of the herniated disc that is pressing on the nerve.
- Laminectomy/Foraminotomy: The surgeon removes a small piece of bone (lamina or bone spur) to create more space for the nerve.
- Spinal Fusion: After removing a disc, the surgeon may fuse two or more vertebrae together to provide stability. This is becoming less common as disc replacement technology improves.
How Can I Prevent a Pinched Nerve from Coming Back?
Prevention is the best medicine. To reduce your risk of recurrence, focus on:
- Maintaining a Healthy Weight: Reduces the overall load on your spine.
- Regular Exercise: Keep your core and back muscles strong and flexible.
- Good Posture: Be mindful of your posture during all activities.
- Ergonomic Workspace: Adjust your chair, desk, and monitor to support a neutral spine.
- Proper Lifting Technique: Always lift with your legs, not your back.
Comparing Pinched Nerve Treatment Options
| Treatment | Best For | How It Works | Evidence Level |
|---|---|---|---|
| Home Care (Rest, Ice/Heat, OTCs) | Mild to moderate symptoms, initial phase. | Reduces acute inflammation and muscle spasm, allows tissues to heal. | High (First-line treatment) |
| Physical Therapy & Exercise | Subacute and chronic symptoms, long-term prevention. | Strengthens supporting muscles, improves flexibility, creates space for the nerve. | High (Strong evidence for radiculopathy) |
| Corticosteroid Injections | Severe, localized pain that limits function. | Delivers potent anti-inflammatory medication directly to the nerve root. | Moderate to High (Effective for short-to-medium term relief) |
| Surgery | Severe, persistent symptoms with neurological deficits failure of conservative care. | Physically removes the source of nerve compression (e.g., disc material, bone spur). | High (For specific, indicated cases) |
Prevalence of Spinal Radiculopathy
While both are common, pinched nerves in the lower back (lumbar radiculopathy) are more prevalent than those in the neck (cervical radiculopathy).
Lumbar issues often stem from the greater mechanical stress placed on the lower spine.
The chart below illustrates the estimated annual incidence, showing how many new cases appear per 100.000 people each year.
Frequently Asked Questions (FAQ) about Pinched Nerves
1. How long does a pinched nerve last?
A mild pinched nerve can resolve within a few days to weeks with proper self-care. More severe cases, especially those involving a herniated disc, can take several months to improve. Chronic cases may persist without targeted treatment.
2. Can a pinched nerve go away on its own?
Yes, many cases of a pinched nerve resolve on their own. The body has a natural ability to heal, and inflammation can subside over time. However, addressing the root cause with posture changes and exercise is key to preventing recurrence.
3. What is the fastest way to heal a pinched nerve?
The fastest approach involves reducing inflammation with rest and ice, followed by gentle movement and stretching to relieve pressure. Correcting posture and avoiding aggravating activities are crucial for rapid recovery. There is no single “magic bullet”.
4. Should I use a chiropractor for a pinched nerve?
Chiropractic care, particularly gentle mobilization and adjustments, can be beneficial for some people. However, high-velocity manipulation should be avoided in acute cases. It’s essential to see a qualified professional who performs a thorough evaluation first.
5. Can massage make a pinched nerve worse?
Deep tissue massage directly over the compressed nerve can sometimes increase inflammation and worsen symptoms. However, gentle massage of the surrounding tight muscles can be very helpful in relieving pressure and is often a component of physical therapy.
6. What sleeping position is best for a pinched nerve in the neck?
Sleeping on your back or side with a supportive pillow that keeps your neck in a neutral alignment is best. Avoid sleeping on your stomach, as this forces your neck into a twisted position for hours.
7. Can stress cause a pinched nerve?
While stress doesn’t directly cause nerve compression, it can contribute significantly. Stress leads to muscle tension, particularly in the neck and shoulders, which can increase pressure on nerves and heighten your perception of pain.
8. Is walking good for a pinched nerve in the back?
Yes, gentle walking is generally excellent for a pinched nerve in the back. It promotes blood flow, prevents stiffness, and engages core muscles without high impact. Listen to your body and avoid walking to the point of significant pain.
Conclusion
Dealing with a pinched nerve in your neck or back can be a painful and frustrating experience, but relief is achievable.
The path to recovery begins with understanding your symptoms and implementing conservative, evidence-based home care strategies like activity modification, targeted exercises and posture correction.
For persistent or severe symptoms, a range of professional treatments from physical therapy to injections and surgery can provide effective relief.
The key is a proactive and patient approach—listening to your body, seeking professional guidance when needed, and committing to preventative habits to protect your spine for the long term.
If you are struggling with persistent pain or neurological symptoms, don’t hesitate to consult a healthcare professional for a personalized diagnosis and treatment plan. Your journey back to a pain-free life starts with taking that first informed step.
Reference
[1] Got a pinched nerve? Strategies and treatments for pain relief
[2] Radiculopathy
https://en.wikipedia.org/wiki/Radiculopathy
[3] https://www.mayoclinic.org/diseases-conditions/pinched-nerve/symptoms-causes/syc-20354746
[4] Exercise training for non-operative and post- …
https://pmc.ncbi.nlm.nih.gov/articles/PMC4616148
[5] https://my.clevelandclinic.org/health/diseases/6481-pinched-nerves
[6] Cervical Radiculopathy – StatPearls
https://www.ncbi.nlm.nih.gov/books/NBK441828
[7] Physical Therapy: An Effective Method For Pinched Nerve …
https://njspine.com/physical-therapy-an-effective-method-for-pinched-nerve-treatment/

