You can effectively lower your A1c levels naturally through a combination of strategic dietary changes, consistent physical activity and targeted lifestyle modifications.
These evidence-based methods focus on improving your body’s insulin sensitivity and overall metabolic health, forming the cornerstone of sustainable blood sugar management.
With over 96 million American adults—more than 1 in 3—having prediabetes according to the CDC, understanding how to manage your A1c is more critical than ever for preventing the progression to type 2 diabetes.
This isn’t just a number on a lab report, it’s a powerful indicator of your long-term health trajectory.
Taking control of your A1c is a proactive step towards reducing the risk of serious complications like heart disease, nerve damage, and vision problems.
In this comprehensive guide, we will move beyond the basics.
We’ll explore the science-backed details of specific exercises, dietary patterns, stress management techniques, and other powerful strategies that can significantly impact your A1c levels.
We will delve into the mechanisms behind why these methods work, providing you with the knowledge and confidence to make lasting changes.
Read on to discover actionable steps you can take today to gain better control over your blood sugar and long-term health.
In This Article
What Is A1c and Why Does It Matter?
Before diving into the strategies for lowering your A1c, it’s essential to understand what this measurement represents and why it’s such a crucial health marker.
Think of it as a long-term report card for your blood sugar, offering a much broader view than a single daily glucose reading.
A Quick Definition of the A1c Test
The A1c test, also known as the hemoglobin A1c, HbA1c, or glycated hemoglobin test, is a simple blood test that measures your average blood glucose (sugar) levels over the past two to three months.
The “glycated” part of the name is key. When sugar circulates in your bloodstream, it naturally attaches, or “glycates”, to hemoglobin, the protein in your red blood cells responsible for carrying oxygen.
Imagine your red blood cells are like tiny sponges traveling through your bloodstream for about three months.
The more sugar there is in your blood over that period, the more sugar will “stick” to these sponges.
The A1c test measures the percentage of your red blood cells that have become sugar-coated.
A higher percentage indicates higher average blood sugar levels during that time frame.
According to leading health organizations like the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the American Diabetes Association (ADA), this test is a primary tool for both diagnosing and monitoring prediabetes and type 2 diabetes because it provides a stable, long-term picture of glycemic control, unaffected by short-term fluctuations from a recent meal or exercise session.
Understanding Your A1c Results
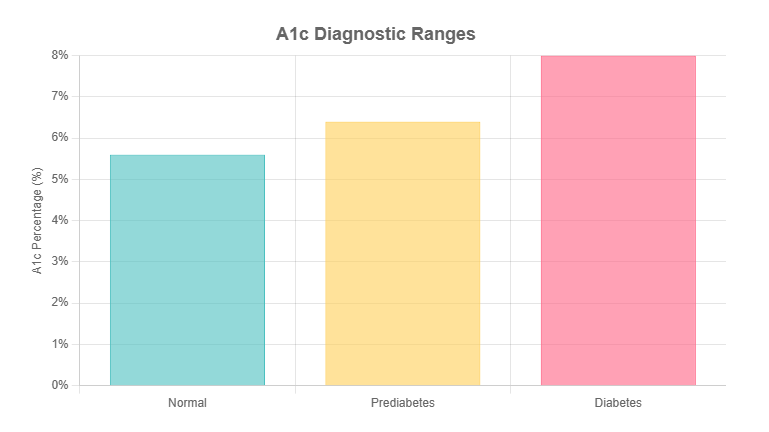
Your A1c result is given as a percentage. This number places you into one of three categories: normal, prediabetes, or diabetes.
Understanding where you fall is the first step toward taking appropriate action.
| A1c Level | Diagnosis |
|---|---|
| Below 5.7% | Normal |
| 5.7% to 6.4% | Prediabetes |
| 6.5% or above | Diabetes |
- Normal (Below 5.7%): Your blood sugar levels have been in a healthy range over the past few months. This is the target for individuals without diabetes.
- Prediabetes (5.7% to 6.4%): This range acts as a critical warning sign. Your blood sugar levels are higher than normal but not yet high enough to be diagnosed as type 2 diabetes. It indicates an increased risk of developing diabetes, heart disease and stroke. The good news is that with lifestyle changes, progression to diabetes can often be prevented or delayed.
- Diabetes (6.5% or above): A result in this range, typically confirmed with a second test, indicates a diagnosis of diabetes. This means your body either isn’t producing enough insulin or isn’t using it effectively, leading to chronically high blood sugar levels.
Your doctor might also discuss your eAG, or estimated Average Glucose.
This simply translates your A1c percentage into the same units (mg/dL or mmol/L) that you see on a home blood glucose meter.
For example, an A1c of 7.0% corresponds to an eAG of about 154 mg/dL.
This can make the long-term average more relatable to the daily numbers you might be tracking.
How Can You Lower Your A1c with Diet?
Diet is arguably the most powerful tool in your arsenal for naturally lowering your A1c.
The food you eat directly impacts your blood sugar levels, and making strategic, consistent changes can lead to profound improvements in your metabolic health.
The goal is not to follow a restrictive, joyless diet, but to adopt a sustainable eating pattern that nourishes your body and helps it manage glucose more effectively.
Prioritize Fiber: The Unsung Hero of Blood Sugar Control
If there’s one nutrient to focus on for A1c management, it’s fiber.
Fiber is a type of carbohydrate that your body can’t digest.
Instead of being broken down into sugar, it passes through your system, providing a host of benefits.
For blood sugar control, soluble fiber is particularly important.
The mechanism is simple yet effective: soluble fiber dissolves in water to form a gel-like substance in your digestive tract.
This gel slows down the digestion and absorption of other carbohydrates, which prevents the rapid, sharp spikes in blood sugar that can elevate your A1c over time.
The American Heart Association recommends adults aim for 25 to 38 grams of fiber per day, a target most Americans fail to meet.
Key Sources of Dietary Fiber:
- Soluble Fiber Sources: These are your best friends for blunting blood sugar spikes. Excellent sources include oats, barley, beans, lentils, apples, citrus fruits, carrots and psyllium husk. Starting your day with a bowl of oatmeal or adding a cup of beans to your soup are easy ways to boost your intake.
- Insoluble Fiber Sources: This type of fiber doesn’t dissolve in water but adds bulk to your stool, promoting regularity. While its direct effect on blood sugar is less pronounced, it’s crucial for digestive health. Find it in whole-wheat flour, wheat bran, nuts, seeds, and vegetables like cauliflower and green beans.
Master Carbohydrate Quality, Not Just Quantity
The conversation around carbohydrates and diabetes has often been oversimplified to “avoid carbs”.
A more effective and sustainable approach is to focus on smart-carbs.
The quality of the carbohydrate you eat matters more than the sheer quantity.
This is where understanding the Glycemic Index (GI) and Glycemic Load (GL) becomes useful.
- The Glycemic Index (GI) is a scale from 0 to 100 that ranks carbohydrate-containing foods by how quickly they cause your blood sugar to rise. High-GI foods (like white bread, sugary cereals, and potatoes) are digested quickly, causing a rapid spike. Low-GI foods (like lentils, non-starchy vegetables, and whole grains) are digested slowly, leading to a more gradual, gentle rise in blood sugar.
- The Glycemic Load (GL) takes this a step further by considering the portion size. It gives a more accurate picture of a food’s real-world impact on your blood sugar.
You don’t need to obsessively calculate numbers.
The key takeaway is to build your meals around low-GI, high-fiber carbohydrates.
Swap white rice for quinoa or brown rice, choose whole-grain bread over white, and fill your plate with colorful, non-starchy vegetables.
Expert Tip: Never eat a “naked” carb. Pairing a carbohydrate with a source of protein or healthy fat can significantly slow its absorption and blunt the blood sugar response. For example, instead of eating an apple by itself, have it with a handful of almonds or a spoonful of peanut butter. This simple trick helps stabilize your energy and your A1c.
Adopt a Proven Eating Pattern: The Mediterranean Diet
Instead of focusing on individual nutrients, adopting a whole eating pattern can be more effective.
The Mediterranean diet is consistently recommended for diabetes management and heart health and for good reason.
It’s not a “diet” in the restrictive sense but a lifestyle centered on whole, nutrient-dense foods.
The core components of a Mediterranean eating pattern include:
- Abundant Vegetables and Fruits: The foundation of the diet, providing fiber, vitamins and antioxidants.
- Healthy Fats: Emphasis on monounsaturated fats from olive oil, avocados, nuts and seeds.
- Lean Proteins: Frequent consumption of fish and poultry, with limited red meat.
- Whole Grains: Foods like farro, barley, and whole-wheat bread are preferred over refined grains.
- Legumes: Beans, lentils, and chickpeas are staples, offering both protein and soluble fiber.
Research has consistently shown that this dietary pattern can improve glycemic control and lower A1c levels.
A meta-analysis published in Diabetes Care found that adherence to a Mediterranean diet was associated with significant improvements in A1c, making it a powerful, evidence-based strategy for long-term health.
The Power of Portion Control and Mindful Eating
Even when eating healthy foods, quantity matters.
Overeating, even healthy foods, can lead to weight gain and higher blood sugar.
This is where portion control and mindful eating come into play.
A simple and effective tool is the Diabetes Plate Method.
It provides a visual guide for building a balanced meal without complicated counting:
- Fill half your plate with non-starchy vegetables (e.g., broccoli, spinach, bell peppers, salad greens).
- Fill one-quarter of your plate with a lean protein source (e.g., chicken, fish, tofu, beans).
- Fill the final quarter of your plate with high-fiber carbohydrates (e.g., quinoa, brown rice, sweet potato, whole-grain pasta).
Beyond what’s on your plate, how you eat is also important.
Mindful eating involves paying full attention to your meal, which can help you better recognize your body’s hunger and fullness cues. Try these tips:
- Use smaller plates: This can trick your brain into feeling satisfied with smaller portions.
- Eat slowly and chew thoroughly: It takes about 20 minutes for your brain to register that you’re full.
- Avoid distractions: Turn off the TV and put away your phone during meals to focus on your food.
What Is the Best Exercise to Lower A1c?
If diet is the fuel, exercise is the engine that helps your body use that fuel efficiently.
Physical activity is a non-negotiable component of any plan to lower A1c.
Its benefits are twofold: it has an immediate effect on blood sugar and a long-term effect on how your body manages glucose.
The Undeniable Impact of Regular Movement
When you exercise, your muscles need energy.
To get this energy, they pull glucose from your bloodstream, which directly lowers your blood sugar levels.
This effect can last for up to 24 hours after a workout.
More importantly, regular exercise makes your body’s cells more sensitive to insulin.
This means your body needs less insulin to do its job, which is the very definition of improved metabolic health and a key factor in lowering your A1c.
The American Diabetes Association recommends that most adults with type 2 diabetes engage in at least 150 minutes of moderate-to-vigorous intensity aerobic exercise per week, spread over at least three days, with no more than two consecutive days without activity.
The Winning Combination: Aerobic and Resistance Training
While any movement is better than none, research has shown that a specific combination of exercise yields the best results for A1c reduction.
While aerobic exercise (cardio) is excellent for heart health and burning calories, and resistance training is crucial for building muscle, doing both is the gold standard.
A landmark study called HART-D (Health Benefits of Aerobic and Resistance Training in individuals with type 2 Diabetes), published in the Journal of the American Medical Association (JAMA), provided definitive evidence.
The study compared four groups: a control group, an aerobic-only group, a resistance-only group, and a group that did a combination of both.
The results were clear: the combination training group achieved the greatest improvement, with a statistically significant A1c reduction of -0.34% compared to the control group. This was a greater reduction than that seen in either the aerobic-only or resistance-only groups, even though all exercise groups spent a similar amount of time working out each week.
This highlights that the synergy between the two types of exercise provides a superior metabolic benefit. Here’s how to incorporate both:
- Aerobic Exercise: This is any activity that raises your heart rate and makes you breathe harder. Aim for at least 30 minutes on most days of the week.
- Examples: Brisk walking, jogging, cycling (outdoors or stationary), swimming, dancing or using an elliptical machine.
- Resistance Training: This involves working your muscles against a force. Building more muscle is metabolically beneficial because muscle tissue uses more glucose than fat tissue, even at rest. Aim for 2-3 non-consecutive days per week.
- Examples: Lifting free weights, using weight machines at a gym, working with resistance bands, or performing bodyweight exercises like squats, push-ups, lunges and planks.
Don’t Underestimate “Exercise Snacks” and Reducing Sedentary Time
The modern lifestyle often involves long periods of sitting, which is detrimental to metabolic health.
Even if you have a dedicated workout session, being sedentary for the rest of the day can counteract some of the benefits.
The solution is to break up prolonged sitting with “exercise snacks”.
Research has shown that even short bouts of light activity can significantly improve post-meal glucose levels.
A study in Diabetes Care found that taking a brief walk every 30 minutes was more effective at lowering post-meal blood sugar than one longer, continuous walk.
The goal is to avoid being stationary for more than 30-60 minutes at a time.
Here are some practical ways to incorporate more movement into your day:
- Set a timer to get up and walk around for 5 minutes every hour.
- Take the stairs instead of the elevator.
- Pace around while talking on the phone.
- Do a set of 10 squats or calf raises while waiting for your coffee to brew.
- Park further away from the entrance at the grocery store.
These small, consistent efforts add up and play a significant role in your overall activity level and, consequently, your A1c.
How Does Weight Loss Affect Your A1c?
For individuals carrying excess weight, weight management is a cornerstone of lowering A1c.
The connection is direct and scientifically proven: losing weight can dramatically improve your body’s ability to manage blood sugar.
The Science: Why Losing Weight Lowers A1c
Excess body fat, particularly visceral fat—the fat stored deep within the abdominal cavity around your organs—is a major contributor to insulin resistance.
This type of fat is metabolically active and releases inflammatory substances that interfere with insulin’s ability to do its job.
When your cells become resistant to insulin, your pancreas has to work overtime to produce more of it to keep blood sugar in check.
Eventually, it can’t keep up, leading to higher blood sugar levels and an elevated A1c.
When you lose weight, you reduce the amount of visceral fat.
This decreases inflammation and allows your cells to become more sensitive and responsive to insulin again.
With improved insulin sensitivity, your body can effectively move glucose from the blood into the cells for energy, resulting in lower average blood sugar and a healthier A1c.
A Realistic Goal: The Power of 5-10%
The prospect of weight loss can feel daunting, but the good news is that you don’t need to achieve a dramatic transformation to see significant metabolic benefits.
The focus should be on modest, sustainable weight loss.
Extensive research, including findings from the landmark Diabetes Prevention Program, has shown that losing just 5% to 10% of your starting body weight can have a massive impact.
One study highlighted by WebMD found that people with type 2 diabetes who lost 5-10% of their body weight were three times as likely to lower their A1c by 0.5%.
A Practical Example: For a person who weighs 200 pounds (91 kg), a 5-10% weight loss translates to just 10-20 pounds (4.5-9 kg). Losing this relatively small amount of weight is often enough to significantly improve A1c levels, reduce the need for medication, and in some cases of prediabetes, even reverse the condition entirely.
This realistic and achievable goal can be a powerful motivator.
It shifts the focus from an intimidating number on the scale to a tangible target that brings profound health rewards.
This level of weight loss is best achieved through the combined diet and exercise strategies discussed in this guide, creating a synergistic effect on your A1c.
Can Better Sleep Really Lower Your A1c?
In the quest to lower A1c, diet and exercise often take center stage, but an equally critical, and often overlooked, factor is sleep.
The quantity and quality of your sleep have a profound impact on your hormones, metabolism and blood sugar regulation.
The Hormonal Connection: Sleep Deprivation and Insulin Resistance
When you don’t get enough quality sleep, your body’s hormonal balance is thrown into disarray.
This has a direct effect on your blood sugar management:
- Increased Cortisol: Sleep deprivation is a physiological stressor that causes your body to release more cortisol, the primary stress hormone. As discussed later, cortisol signals your liver to release more glucose into the bloodstream, leading to higher blood sugar levels.
- Decreased Insulin Sensitivity: Even a single night of poor sleep can make your cells more resistant to insulin the next day. This means your pancreas has to pump out more insulin to manage the same amount of glucose, putting a strain on your system.
- Appetite Dysregulation: Lack of sleep also affects the hormones that control hunger and fullness. It increases ghrelin (the “hunger hormone”) and decreases leptin (the “satiety hormone”), leading to increased cravings for high-carb, sugary foods, which further complicates blood sugar control.
The scientific evidence is compelling. A study published in the Chinese Medical Journal found a clear association between sleep disorders, such as obstructive sleep apnea and poor sleep quality and higher A1c levels in patients with type 2 diabetes.
The study concluded that poor diabetes control is an important factor that disturbs sleep, and conversely, sleep disturbances negatively affect diabetes control, creating a vicious cycle.
Actionable Tips for Improving Sleep Quality
Prioritizing sleep is a non-negotiable strategy for improving your A1c.
The goal is to get 7-9 hours of quality, uninterrupted sleep per night. This involves practicing good “sleep hygiene”.
Featured Snippet: How to Improve Sleep for Better Blood Sugar
- Stick to a consistent sleep schedule: Go to bed and wake up around the same time every day, even on weekends. This helps regulate your body’s internal clock.
- Create a restful environment: Your bedroom should be cool, dark, and quiet. Use blackout curtains, an eye mask, or a white noise machine if needed.
- Avoid stimulants late in the day: Steer clear of caffeine and nicotine in the afternoon and evening, as their effects can last for hours.
- Limit large meals and alcohol before bed: A heavy meal can cause indigestion, and while alcohol might make you feel sleepy initially, it disrupts sleep later in the night.
- Power down screens: The blue light emitted from phones, tablets, and computers can suppress melatonin production, the hormone that signals your body it’s time to sleep. Stop using screens at least an hour before bed.
- Establish a relaxing pre-sleep routine: Signal to your body that it’s time to wind down. This could include taking a warm bath, reading a book (a physical one!), listening to calm music, or practicing gentle stretching.
What Is the Link Between Stress and High A1c?
The mind-body connection is powerful, and nowhere is this more evident than in the relationship between stress and blood sugar.
Chronic stress can sabotage even the best diet and exercise efforts, making it a critical factor to address when trying to lower your A1c.
How Stress Directly Raises Your Blood Sugar
Your body’s reaction to stress is a primal survival mechanism known as the “fight or flight” response.
When you perceive a threat—whether it’s a physical danger or a psychological pressure like a work deadline or financial worry—your adrenal glands release a flood of stress hormones, primarily cortisol and adrenaline.
These hormones have a direct impact on your blood sugar.
They signal your liver and muscles to release stored glucose (in the form of glycogen) into the bloodstream.
The purpose of this is to provide a quick burst of energy for your muscles to either fight the threat or flee from it.
In an acute situation, this is helpful. However, in our modern world, many stressors are chronic and psychological rather than short-lived and physical.
When you are under chronic stress, your cortisol levels remain persistently elevated.
This leads to a constant, slow release of glucose from your liver, resulting in chronically higher blood sugar levels.
Over time, this contributes directly to a higher A1c.
Furthermore, stress can also lead to unhealthy coping behaviors like emotional eating, skipping workouts, and poor sleep, all of which further exacerbate the problem.
Effective Stress-Management Techniques
Managing stress is not about eliminating it entirely—an impossible task—but about improving your response to it.
A review on the link between stress and A1c in the journal Current Diabetes Reports found that interventions targeting stress management can lead to modest but significant improvements in A1c.
Incorporating relaxation practices into your routine can help lower cortisol levels and improve your overall metabolic health.
Here are some evidence-based techniques to consider:
- Mindfulness Meditation: This practice involves focusing on your breath and observing your thoughts without judgment. Apps like Headspace and Calm can guide you through sessions. Even 10 minutes a day can reduce stress and improve your physiological response.
- Deep Breathing Exercises: Simple techniques like diaphragmatic breathing (belly breathing) can activate the parasympathetic nervous system, which promotes a state of rest and calm. Try inhaling slowly for four counts, holding for four, and exhaling for six.
- Yoga and Tai Chi: These mind-body practices combine physical postures, breathing exercises, and meditation. They are excellent for reducing stress while also providing the benefits of light physical activity.
- Regular Physical Activity: Exercise is one of the most effective stress relievers. It serves a dual purpose by directly lowering blood sugar and also burning off excess stress hormones.
- Spending Time in Nature: Research shows that even short periods spent in natural environments can lower cortisol levels and reduce feelings of stress.
Should You Consider Supplements to Lower A1c?
The supplement aisle is filled with products promising to lower blood sugar and improve A1c.
While the idea of a “magic pill” is appealing, it’s crucial to approach this area with caution, skepticism and a strong focus on evidence.
Lifestyle changes are the foundation of A1c management and no supplement can replace them.
A Word of Caution: Supplements Are Not a Magic Bullet
Important Disclaimer: Always consult your doctor or a registered dietitian before starting any new supplement. Many supplements can interact with prescription medications (especially diabetes medications), have side effects, or may not be appropriate for individuals with certain health conditions, such as kidney disease. The supplement industry is not as tightly regulated as the pharmaceutical industry, so product quality and purity can vary.
Supplements should be viewed as a potential *complement* to a solid foundation of diet, exercise and stress management, not a substitute for it.
The evidence for many supplements is often preliminary, based on small studies, or inconsistent.
Examining the Evidence for Popular Supplements
With that crucial disclaimer in mind, some supplements have shown more promise than others in scientific research.
Here is a balanced look at a few of the most commonly discussed options:
- Berberine: This is a compound extracted from several different plants. It has gained significant attention because some research suggests it can be remarkably effective at lowering blood sugar. A meta-analysis of studies found that berberine could significantly lower fasting blood glucose, post-meal glucose, and A1c. Some studies have even found its effects to be comparable to oral diabetes drugs like metformin. However, it can cause digestive side effects, and more long-term safety data is needed.
- Cinnamon: This common spice contains compounds that may improve insulin sensitivity and slow the breakdown of carbohydrates in the digestive tract. While some studies have shown modest benefits in lowering fasting blood sugar and A1c, the results are mixed. The effectiveness can depend heavily on the type of cinnamon (Cassia vs. Ceylon) and the dosage. It’s safe to use as a spice in your food, but high-dose supplements should be discussed with a doctor.
- Magnesium: This essential mineral plays a crucial role in over 300 enzymatic reactions in the body, including glucose metabolism and insulin signaling. A deficiency in magnesium is strongly linked to insulin resistance and an increased risk of type 2 diabetes. If a blood test reveals you are deficient, supplementation may help improve your insulin sensitivity and glycemic control. However, if your levels are already adequate, more is not necessarily better. Good food sources include leafy greens, nuts, seeds, and dark chocolate.
- Alpha-Lipoic Acid (ALA): A powerful antioxidant, ALA has been studied for its potential to improve insulin sensitivity and reduce symptoms of diabetic neuropathy (nerve pain). Some research indicates it may have a modest effect on lowering A1c.
The bottom line on supplements is to be an informed consumer.
Do your research from reliable sources, prioritize those with human clinical trials, and always, always have a conversation with your healthcare provider first.
Putting It All Together: Your 3-Month Action Plan
Knowledge is power, but action is what creates change. Lowering your A1c is a journey that happens over months, not days.
Since the A1c test reflects a 3-month average, this is the perfect timeframe for a focused action plan.
Here is a step-by-step guide to help you build sustainable habits.
Month 1: Building the Foundation
The first month is about awareness and incorporating small, manageable changes.
The goal is to build momentum without feeling overwhelmed.
- Week 1: Track and Assess. Start a food and activity log. Use a notebook or an app to write down everything you eat and any physical activity you do. Don’t judge, just observe. This will give you a baseline and reveal patterns you may not have noticed.
- Week 2: Focus on Movement. Aim for a 30-minute brisk walk 3-4 times this week. If that’s too much, start with 15 minutes. The goal is to establish a routine. Also, practice “exercise snacks”: get up and move for 5 minutes every hour.
- Week 3: Add Fiber and Vegetables. Make one simple dietary change: add one serving of non-starchy vegetables (like a side salad or steamed broccoli) to every dinner. Also, try swapping one refined grain (like white bread) for a whole-grain alternative.
- Week 4: Hydrate and Plan. Focus on drinking enough water throughout the day. Aim for about 8 glasses. Use this week to plan your meals for the following week, ensuring you have healthy ingredients on hand.
Month 2: Increasing Intensity and Consistency
With a foundation in place, month two is about ramping up your efforts and making your new habits more consistent.
- Week 5: Increase Exercise Intensity. Increase your aerobic exercise to the recommended 150 minutes per week (e.g., 30 minutes, 5 days a week). Push yourself to walk a little faster or try a new activity like cycling.
- Week 6: Introduce Resistance Training. Incorporate two days of resistance training. This can be simple bodyweight exercises at home (squats, lunges, push-ups) or a session at the gym. Focus on proper form.
- Week 7: Master the Plate Method. For every lunch and dinner this week, consciously build your plate according to the Diabetes Plate Method (1/2 veggies, 1/4 protein, 1/4 fiber-rich carbs).
- Week 8: Tackle Sleep. Make sleep a priority. Implement at least two sleep hygiene tips from the guide, such as setting a consistent bedtime and avoiding screens for an hour before bed.
Month 3: Fine-Tuning and Lifestyle Integration
The final month is about solidifying your habits for the long term and addressing the more nuanced aspects of health.
- Week 9: Manage Stress. Dedicate 10 minutes every day to a stress-management practice. This could be guided meditation, deep breathing exercises, or journaling. Notice how it affects your mood and food choices.
- Week 10: Review and Refine. Look back at your food and activity logs. What’s working well? Where are the challenges? Identify one specific area to improve, such as reducing sugary drinks or late-night snacking.
- Week 11: Experiment with Recipes. To keep things interesting, try two new healthy recipes this week. Focus on meals that are rich in fiber and lean protein.
- Week 12: Celebrate and Re-test. Acknowledge your hard work and consistency over the past three months. Schedule a follow-up appointment with your doctor to discuss your progress and get your A1c re-tested. The results will provide valuable feedback and motivation to continue your healthy lifestyle.
Frequently Asked Questions (FAQ)
1. How quickly can I lower my A1c?
You can start seeing improvements in your daily blood sugar within weeks, but since the A1c test measures a 2-3 month average, it typically takes that long to see a significant change in your score. Consistency with diet and exercise is the most important factor for rapid improvement.
2. What one food lowers A1c the most?
No single food works like magic. However, foods high in soluble fiber, such as beans, lentils, oats, and barley, have a powerful and proven effect on slowing sugar absorption and improving glycemic control, making them top contenders for impacting your A1c.
3. Can drinking water lower my A1c?
Yes, indirectly. Staying well-hydrated helps your kidneys function optimally to flush out excess sugar through urine. It also supports overall metabolic function and can prevent dehydration-induced rises in blood sugar concentration, contributing to a lower A1c over time.
4. Does intermittent fasting help lower A1c?
Some research suggests that intermittent fasting can improve insulin sensitivity and lead to weight loss, both of which can help lower A1c. However, it’s not suitable for everyone, especially those on certain diabetes medications. Always consult a doctor before trying it.
5. Can I lower my A1c by 1 point in 3 months?
Yes, lowering your A1c by a full percentage point (e.g., from 7.5% to 6.5%) in three months is an achievable goal for many people, but it typically requires aggressive and highly consistent changes in diet, exercise, and weight management. Individual results will vary.
6. What fruits should I avoid to lower my A1c?
No fruit needs to be completely avoided. The key is portion control and pairing. Berries, apples, and pears are excellent low-GI choices. It’s best to eat whole fruit rather than drinking juice and to pair fruit with a protein or fat source (like nuts) to blunt the sugar spike.
7. Is an A1c of 5.7 dangerous?
An A1c of 5.7% is the threshold for a prediabetes diagnosis. While not immediately dangerous, it is a critical warning sign that your body is struggling to manage blood sugar. It signals a high risk for developing type 2 diabetes and is a crucial prompt to make proactive lifestyle changes.
8. Does apple cider vinegar really lower A1c?
Some small studies suggest apple cider vinegar may modestly lower post-meal blood sugar by slowing stomach emptying. However, it is not a proven treatment for lowering long-term A1c and should not replace evidence-based strategies. Use it in moderation, diluted in water.
9. What is a normal A1c level by age?
The definition of a normal A1c level (below 5.7%) does not typically change with age. However, for individuals already diagnosed with diabetes, a doctor might set a less strict A1c target (e.g., below 8.0%) for older adults, especially if they have other health conditions or a risk of hypoglycemia.
Conclusion
Lowering your A1c naturally is not about a quick fix or a period of deprivation, it is about building a sustainable, healthier lifestyle.
As we’ve explored, this is a holistic endeavor that is well within your reach.
The journey rests on a powerful trifecta of evidence-based strategies: nourishing your body with a fiber-rich, whole-foods diet, committing to a consistent routine of both aerobic and resistance exercise and managing the often-underestimated pillars of health—sleep and stress.
Each of these components works in synergy to improve your body’s insulin sensitivity and overall metabolic function.
The path to a lower A1c is paved with small, consistent choices that accumulate over time to produce profound results.
This is an empowering process that puts you in the driver’s seat of your long-term health.
Take the first step today. Don’t feel you have to change everything at once. Choose one strategy from this guide—like adding a 20-minute walk after dinner or swapping your morning pastry for a bowl of oatmeal—and commit to it for one week. Small wins build momentum for lasting change. Your future self will thank you.
Medical Disclaimer
The information in this article is for educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.