Alzheimer’s disease is a progressive brain disorder that gradually destroys memory, thinking skills, and eventually, the ability to carry out the simplest tasks. Its early signs are often subtle and easily dismissed as normal aging.
This reality underscores a critical public health challenge: an estimated 7.2 million Americans age 65 and older are projected to be living with Alzheimer’s in 2025, a number expected to nearly double by 2060 without medical breakthroughs. The urgent need for early recognition has never been greater.
Understanding the nuances of this disease is the first step toward empowerment.
This guide offers a comprehensive exploration of Alzheimer’s, moving beyond surface-level descriptions.
We will conduct a deep dive into the 10 classic warning signs, uncover the often-overlooked subtle symptoms that may appear first, and provide a clear framework for distinguishing between Alzheimer’s and the normal cognitive changes of aging.
Furthermore, we will examine the latest 2024 updates on risk factors and groundbreaking treatments that are changing the landscape of care.
Arming yourself with this knowledge is a vital act of care for yourself and your loved ones.
In Thie Article
Part 1: Understanding Alzheimer’s: More Than Just Memory Loss
Before we can identify the early signs of Alzheimer’s, it is essential to establish a clear foundational understanding of what the disease is—and what it is not.
The terms “dementia” and “Alzheimer’s” are often used interchangeably, but they represent different concepts.
Clarifying this distinction is the first step toward a more precise comprehension of the condition.
What is the Difference Between Alzheimer’s and Dementia?
Think of dementia as an umbrella term. It is not a specific disease but rather a general term for a decline in mental ability—such as memory loss, language difficulties, and impaired reasoning—that is severe enough to interfere with daily life.
There are many different conditions that can cause dementia, including vascular dementia, Lewy body dementia and frontotemporal dementia.
Alzheimer’s disease is the most common cause of dementia.
According to the Alzheimer’s Association, it accounts for an estimated 60% to 80% of all dementia cases.
Therefore, while everyone with Alzheimer’s has dementia, not everyone with dementia has Alzheimer’s disease. Identifying the specific cause of dementia is crucial because it affects prognosis, management and potential treatment options.
What Happens to the Brain in Alzheimer’s Disease?
At its core, Alzheimer’s is a physical disease that causes brain cells to degenerate and die.
This process is associated with two hallmark pathological changes in the brain, which scientists believe disrupt communication between neurons and interfere with cellular processes.
- Plaques: These are microscopic clumps of a protein fragment called beta-amyloid. In a healthy brain, these fragments are broken down and eliminated. In Alzheimer’s disease, they accumulate to form hard, insoluble plaques that build up in the spaces between nerve cells, disrupting cell-to-cell communication.
- Tangles: These are twisted fibers of another protein called tau. In a healthy brain, tau proteins help stabilize microtubules, which are part of the cell’s internal transport system for carrying nutrients. In Alzheimer’s, tau proteins change shape, collapse into twisted strands and form tangles inside the brain cells. This disables the transport system and leads to cell death.
A critical point to understand is that these pathological changes begin to develop in the brain long before the first signs of memory loss become apparent—often a decade or more.
This “preclinical” stage of Alzheimer’s is a major focus of current research, as intervening during this window may offer the best chance to slow or prevent the disease’s progression.
Part 2: The Core Focus: Recognizing the 10 Early Warning Signs of Alzheimer’s
The Alzheimer’s Association has identified ten key warning signs that can help individuals and families recognize the potential onset of the disease.
It’s important to note that experiencing one sign does not automatically mean a person has Alzheimer’s.
However, if multiple signs are present and represent a change from a person’s usual behavior, it is a strong signal to consult a healthcare professional.
Here, we explore each sign in detail, contrasting it with typical age-related changes.
1. Memory Loss That Disrupts Daily Life
This is the most widely recognized symptom of Alzheimer’s. It goes far beyond occasional forgetfulness.
It involves forgetting recently learned information, important dates, or events, and repeatedly asking for the same information.
There is often an increasing reliance on memory aids (e.g., reminder notes, electronic devices) or family members for things the person used to handle on their own.
- Sign of Alzheimer’s: Forgetting a recent, significant conversation or event entirely and not recalling it later, even when prompted.
- Typical Age-Related Change: Sometimes forgetting names or appointments but remembering them later. For example, you might forget where you put your keys but can retrace your steps to find them.
2. Challenges in Planning or Solving Problems
Some individuals may experience changes in their ability to develop and follow a plan or work with numbers.
This can manifest as difficulty following a familiar recipe that they have used for years or trouble keeping track of monthly bills.
Concentration may become difficult, and tasks may take much longer to complete than before.
- Sign of Alzheimer’s: A sudden and consistent inability to manage a monthly budget or balance a checkbook, tasks that were previously routine.
- Typical Age-Related Change: Making an occasional error when balancing a checkbook.
3. Difficulty Completing Familiar Tasks
People with early Alzheimer’s often find it hard to complete daily tasks that were once second nature.
They might have trouble driving to a familiar location, like the grocery store they’ve visited for 20 years, or forget the rules of a favorite game.
The difficulty is not due to physical inability but a cognitive breakdown in the sequence of steps required.
- Sign of Alzheimer’s: Getting lost on the way to a friend’s house they have visited countless times or being unable to operate a familiar appliance like a microwave.
- Typical Age-Related Change: Occasionally needing help to use the settings on a new or complex appliance.
4. Confusion with Time or Place
Losing track of dates, seasons, and the general passage of time is a common sign.
Individuals with Alzheimer’s may forget where they are or how they got there.
They may have difficulty understanding something that is not happening in the immediate present, struggling with concepts of “yesterday” or “next week”.
- Sign of Alzheimer’s: Believing it is a different year, or being unsure of the current season.
- Typical Age-Related Change: Forgetting what day of the week it is for a moment but figuring it out later.
5. Trouble Understanding Visual Images and Spatial Relationships
For some, vision problems are a sign of Alzheimer’s.
This is not about eyesight in the traditional sense (e.g., needing glasses).
It’s about the brain’s ability to interpret what the eyes see.
This can lead to difficulty with reading, judging distance and determining color or contrast.
These spatial issues can make activities like driving or navigating stairs particularly dangerous.
- Sign of Alzheimer’s: Misjudging the distance to a curb, leading to stumbles, or having trouble distinguishing between similar colors.
- Typical Age-Related Change: Vision changes related to cataracts or other age-related eye conditions.
6. New Problems with Words in Speaking or Writing
People with Alzheimer’s may have trouble following or joining a conversation.
They might stop in the middle of a sentence and have no idea how to continue or they may repeat themselves.
They often struggle with vocabulary, have problems finding the right word, or call things by the wrong name (e.g., calling a “watch” a “hand-clock”).
- Sign of Alzheimer’s: Consistently struggling to find common words to the point that it makes conversation difficult to follow.
- Typical Age-Related Change: Sometimes having trouble finding the right word but being able to describe it or eventually recall it.
7. Misplacing Things and Losing the Ability to Retrace Steps
A person with Alzheimer’s disease may put things in unusual places—for instance, placing car keys in the refrigerator or a wallet in the sugar bowl.
More importantly, they lose the ability to go back over their steps to find the misplaced item.
As the disease progresses, they may accuse others of stealing the items they cannot find.
- Sign of Alzheimer’s: Frequently misplacing items in illogical locations and being unable to find them.
- Typical Age-Related Change: Misplacing things from time to time and being able to retrace steps to locate them.
8. Decreased or Poor Judgment
Individuals may experience changes in judgment or decision-making.
This can manifest in various ways, such as making poor financial decisions (e.g., giving large sums of money to telemarketers) or paying less attention to personal hygiene and grooming.
They may make choices that are out of character and seem to lack common sense.
- Sign of Alzheimer’s: A noticeable decline in personal grooming habits or repeatedly falling for obvious scams.
- Typical Age-Related Change: Making a questionable decision once in a while, like forgetting to get an oil change for the car.
9. Withdrawal from Work or Social Activities
A person with Alzheimer’s may start to remove themselves from hobbies, social activities, work projects or sports.
They may have trouble keeping up with a favorite team or remembering how to complete a beloved hobby.
The cognitive challenges can make social interaction stressful and exhausting, leading them to avoid situations they once enjoyed.
- Sign of Alzheimer’s: Giving up a lifelong hobby like bridge or knitting because they can no longer follow the rules or patterns.
- Typical Age-Related Change: Sometimes feeling weary of work or social obligations and wanting a break.
10. Changes in Mood and Personality
The mood and personality of someone with Alzheimer’s can change significantly.
They can become confused, suspicious, depressed, fearful or anxious.
They may be easily upset at home, at work, with friends, or in places where they are out of their comfort zone.
This is often a direct result of the confusion and memory loss they are experiencing.
- Sign of Alzheimer’s: Becoming uncharacteristically suspicious of family members or easily agitated in familiar surroundings.
- Typical Age-Related Change: Developing very specific ways of doing things and becoming irritable when a routine is disrupted.
Part 3: Beyond the Obvious: Subtle Symptoms and Real-World Experiences
While the 10 warning signs provide a crucial framework, the initial presentation of Alzheimer’s can be far more nuanced.
Often, the earliest changes are not the classic memory problems but subtle shifts in personality, motivation and behavior that are easily misinterpreted.
Recognizing these can lead to an earlier diagnosis and intervention.
“My mom’s first sign wasn’t forgetting things,” one caregiver shared on a Reddit forum. “It was that she just… stopped. She stopped gardening, stopped calling her friends, stopped cooking her elaborate Sunday dinners. We thought she was depressed, but it was a total lack of initiative. It was apathy”.
Apathy and Loss of Initiative
Apathy, a lack of interest, enthusiasm, or concern, is one of the most common and persistent neuropsychiatric symptoms in Alzheimer’s disease, yet it is frequently overlooked.
It’s not sadness or depression, but rather an emotional flatness and a loss of “spark”.
A person may seem content to sit and do nothing for hours, not because they are tired, but because they lack the internal drive to initiate an activity.
A once-avid gardener may suddenly lose all interest in their plants, not because they are physically unable, but because they lack the motivation to start.
Anxiety and Depression
New or worsening anxiety and depression in an older adult should always be evaluated carefully.
While these can be standalone conditions, they can also be an early symptom of Alzheimer’s.
The anxiety may stem from a subconscious awareness that something is wrong with their cognitive abilities.
Research published in journals like Neurology has shown a significant link between the onset of depression in late life and an increased risk of developing dementia later on.
Changes in Financial Management
Complex tasks are often the first to be affected, and managing personal finances is a highly complex cognitive activity.
For many families, a pile of unpaid bills, letters from collection agencies, or unusual and extravagant purchases are the first concrete signs that something is seriously wrong.
This goes beyond simply missing a payment, it’s a fundamental breakdown in the ability to understand and manage a budget, write checks correctly or identify and avoid financial scams.
Uncharacteristic Vision Problems
As mentioned in the 10 signs, visual-spatial issues can be an early symptom.
However, these can be more specific and unusual than just “trouble reading”.
Some individuals develop a rare variant of Alzheimer’s known as Posterior Cortical Atrophy (PCA). In PCA, the brain damage is concentrated in the back of the brain (the occipital lobe), which processes visual information.
Early symptoms can include difficulty judging distances, navigating stairs, trouble with hand-eye coordination (like buttoning a shirt) and misinterpreting complex visual scenes.
A person might see a collection of objects on a table but be unable to identify a specific item, like a fork, from the clutter.
Part 4: Normal Aging vs. Alzheimer’s: A Comparative Guide
One of the greatest sources of anxiety for many people as they get older is wondering whether a memory slip is a normal part of aging or a sign of something more serious.
It’s true that our brains change with age, processing speed may slow down, and it might take longer to learn new information.
However, the changes caused by Alzheimer’s disease are of a different nature and magnitude.
This table provides a clear, side-by-side comparison to help distinguish between typical age-related changes and potential signs of Alzheimer’s.
| Typical Age-Related Change | Potential Sign of Alzheimer’s |
|---|---|
| Making a bad decision once in a while. | Making poor judgments and decisions much of the time. |
| Missing a monthly payment. | Inability to manage a budget or pay bills consistently. |
| Forgetting which day it is but remembering later. | Losing track of the date, season or time of year. |
| Sometimes forgetting which word to use. | Difficulty holding or following a conversation. |
| Losing things from time to time. | Misplacing things in unusual places and being unable to retrace steps to find them. |
| Feeling sad or moody occasionally. | Significant changes in mood and personality, such as increased suspicion, fear or anxiety. |
| Finding it harder to multitask. | Struggling to plan or solve problems that were once easy. |
Part 5: The Journey of the Disease: Understanding the Stages of Alzheimer’s
Alzheimer’s disease is progressive, meaning its symptoms develop slowly and worsen over time.
While each person’s journey with the disease is unique, the progression can generally be broken down into several stages.
The most common framework uses a three-stage model, though more detailed seven-stage models (like the Reisberg Scale) are used by clinicians for more granular assessment.
Understanding this progression can help families and caregivers anticipate future needs and plan for care.
The Three-Stage Model
- Early-Stage (Mild) Alzheimer’s: In this stage, a person can often still function independently. They may still drive, work, and be part of social activities. However, they begin to experience memory lapses, such as forgetting familiar words or the location of everyday objects. Friends, family, or the individuals themselves may begin to notice these difficulties.
- Middle-Stage (Moderate) Alzheimer’s: This is typically the longest stage and can last for many years. As the disease progresses, the person with Alzheimer’s will require a greater level of care. Dementia symptoms become more pronounced. They may confuse words, get frustrated or angry, and act in unexpected ways, such as refusing to bathe. Damage to nerve cells in the brain can also make it difficult to express thoughts and perform routine tasks.
- Late-Stage (Severe) Alzheimer’s: In the final stage of the disease, individuals lose the ability to respond to their environment, to carry on a conversation, and, eventually, to control movement. They may still say words or phrases, but communicating pain becomes difficult. As memory and cognitive skills continue to worsen, significant personality changes may take place, and individuals need extensive, round-the-clock assistance with daily personal care.
The timeline for this progression varies significantly.
On average, a person with Alzheimer’s lives four to eight years after diagnosis, but some can live as long as 20 years, depending on age, other health conditions and the quality of care received.
This variability underscores the importance of personalized care planning.
Part 6: Causes, Risks and the Latest 2024 Research
While the exact cause of Alzheimer’s disease remains unknown, scientists believe it is triggered by a combination of genetic, lifestyle, and environmental factors that affect the brain over time.
Research has identified several key risk factors, some of which cannot be changed, while others can be modified to potentially lower one’s risk.
Genetic and Unmodifiable Risk Factors
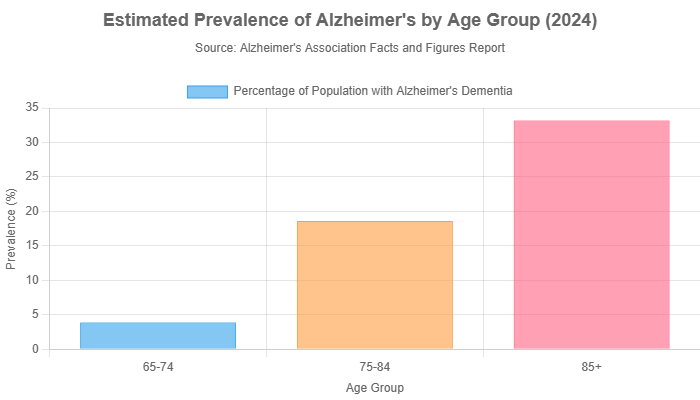
- Age: This is the single greatest known risk factor for Alzheimer’s. The likelihood of developing the disease doubles about every five years after age 65.
- Family History and Genetics: Having a first-degree relative (parent or sibling) with Alzheimer’s increases your risk. This risk is partly related to specific genes. The most common risk gene is a form of the apolipoprotein E gene, known as APOE-e4. While inheriting this gene increases risk, it does not guarantee a person will develop the disease.
The Heart-Head Connection: Modifiable Lifestyle Factors
A growing body of evidence shows a strong connection between the health of your heart and blood vessels and the health of your brain.
Many of the same factors that increase the risk of cardiovascular disease also appear to increase the risk of developing Alzheimer’s. These include:
- High blood pressure (hypertension)
- High cholesterol
- Poorly managed type 2 diabetes
- Smoking
- Obesity
- Lack of regular physical exercise
Managing these conditions through lifestyle changes and medication can play a significant role in maintaining brain health and potentially reducing the risk of dementia.
New Risk Factors Identified in 2024
The field of Alzheimer’s research is constantly evolving. In a landmark 2024 update to its 2020 report, the prestigious Lancet Commission on dementia prevention, intervention and care identified two new modifiable risk factors, further expanding our understanding of how to protect brain health.
- Untreated Vision Loss: The commission added untreated vision impairment in midlife as a significant risk factor. The theory is that sensory deprivation from poor vision can reduce cognitive stimulation and social engagement and may also share common underlying causes with dementia. This highlights the importance of regular eye exams and correcting vision problems.
- High LDL Cholesterol in Midlife: While high cholesterol has long been a known risk, the 2024 report specifically emphasized the danger of high levels of low-density lipoprotein (LDL) or “bad” cholesterol, particularly during midlife (ages 45-65). This reinforces the critical need for early and proactive management of cholesterol levels to protect long-term brain health.
Part 7: Diagnosis and New Hope: Modern Approaches to Treatment
Receiving a timely and accurate diagnosis is the most critical step in managing Alzheimer’s disease.
It opens the door to treatments, support services, and clinical trials, and allows individuals and families to plan for the future.
The diagnostic and treatment landscape has changed more in the last few years than in the preceding decades, offering new hope.
The Diagnostic Process
There is no single test for Alzheimer’s.
A diagnosis is made through a comprehensive medical evaluation to rule out other possible causes of symptoms.
This process typically includes:
- Medical and Family History: A thorough review of current and past health problems, as well as any family history of dementia.
- Cognitive and Neuropsychological Tests: These tests assess memory, problem-solving, attention, language and other thinking skills to identify areas of impairment.
- Neurological Exam: A doctor will assess reflexes, coordination, balance, speech and sensation to rule out other neurological conditions like stroke or Parkinson’s disease.
- Brain Imaging: Structural imaging like MRI or CT scans can identify tumors, evidence of strokes or other abnormalities. Functional imaging like PET scans can show patterns of brain activity or, more recently, visualize the buildup of amyloid plaques and tau tangles in the brain.
- Biomarkers: These are revolutionary tools that can detect the biological signs of Alzheimer’s. Tests on cerebrospinal fluid (CSF) obtained via a spinal tap, or newer blood tests, can measure levels of beta-amyloid and tau proteins, providing direct evidence of the disease pathology.
Modern Treatment Landscape (Updated for 2025)
While there is still no cure for Alzheimer’s, the treatment options have expanded significantly.
They fall into two main categories: those that manage symptoms and those that target the underlying disease process.
Symptomatic Treatments
These medications, such as cholinesterase inhibitors (e.g., donepezil) and memantine, can help temporarily manage memory and thinking problems.
They do not stop the progression of the disease but can improve quality of life for a period of time.
Disease-Modifying Therapies
This is where the most exciting breakthroughs have occurred. A new class of drugs, known as anti-amyloid monoclonal antibodies, has been developed to target and remove beta-amyloid plaques from the brain.
These are the first treatments shown to slow the progression of the disease itself.
- Lecanemab (Leqembi®): Granted full FDA approval in 2023, this intravenous infusion has been shown in clinical trials to moderately slow cognitive and functional decline in people with early-stage Alzheimer’s.
- Donanemab (Kisunla™): This is the newest therapy in this class. Following extensive clinical trials, it received full **FDA approval in July 2024**. Like lecanemab, it is an intravenous infusion designed to remove amyloid plaques.
It is crucial to understand that these disease-modifying therapies are only for individuals in the early stages of Alzheimer’s disease with confirmed amyloid pathology.
They also carry risks, including side effects like brain swelling or bleeding (known as ARIA), and require careful monitoring by a specialist. However, their arrival marks a pivotal new era in the fight against Alzheimer’s.
Part 8: Frequently Asked Questions (FAQ)
At what age do early signs of Alzheimer’s appear?
While Alzheimer’s is most common in people over 65, early-onset Alzheimer’s can affect people in their 40s or 50s. Symptoms typically appear after age 60, but the underlying brain changes can begin years or even decades earlier.
Can stress cause Alzheimer’s?
There is no evidence that stress directly causes Alzheimer’s. However, chronic stress can contribute to risk factors like high blood pressure and inflammation, which are linked to dementia. Managing stress is an important part of a brain-healthy lifestyle.
Is Alzheimer’s hereditary?
Having a parent or sibling with Alzheimer’s increases your risk, but it’s not a guarantee. A small percentage of cases (less than 1%) are caused by specific genetic mutations that are directly inherited. For most people, genetics is just one of several risk factors.
Can you reverse Alzheimer’s?
Currently, there is no way to reverse the brain damage caused by Alzheimer’s. However, new disease-modifying treatments can slow its progression, and lifestyle changes can help manage symptoms and improve quality of life. Early intervention is key.
What is the first memory to go with Alzheimer’s?
The first memories to be affected are typically short-term memories—things that just happened. A person might forget a conversation they had minutes ago or what they ate for breakfast, while still having vivid memories of their childhood.
Does forgetting words mean I have Alzheimer’s?
Not necessarily. Occasional trouble finding the right word is a normal part of aging. The concern with Alzheimer’s is when this problem becomes frequent and severe enough to disrupt conversations, or when a person starts substituting incorrect or nonsensical words.
What is the difference between mild cognitive impairment (MCI) and Alzheimer’s?
MCI is a condition where a person has more memory or thinking problems than normal for their age, but the symptoms are not severe enough to interfere with their daily life. MCI can be a transitional stage to Alzheimer’s, but not everyone with MCI will develop dementia.
What is the latest treatment for Alzheimer’s in 2024?
The latest major treatment to receive FDA approval is Donanemab (brand name Kisunla™), approved in July 2024. It is a disease-modifying therapy that removes amyloid plaques from the brain to slow the progression of early-stage Alzheimer’s disease.
Conclusion
The journey of understanding and confronting Alzheimer’s disease begins with awareness.
Recognizing the early signs—both the classic 10 warnings and the more subtle behavioral shifts—is the first and most powerful step you can take.
Distinguishing these changes from the landscape of normal aging allows for proactive conversations and timely medical consultation.
The landscape of Alzheimer’s is no longer one of passive waiting, it is one of active management and newfound hope.
With the advent of advanced diagnostics and groundbreaking disease-modifying therapies like Lecanemab and Donanemab, the narrative is shifting from inevitable decline to proactive intervention.
These advancements, coupled with a deeper understanding of modifiable risk factors, empower us to take charge of our brain health in a way that was not possible a decade ago.
If you are concerned about your memory or the cognitive health of a loved one, the most important step is to schedule an appointment with a healthcare professional.
Early diagnosis is the key that unlocks access to the full spectrum of support, treatment and resources available.
Do not wait. Your future self, or the future of someone you love, may depend on the action you take today.
We invite you to share your experiences, questions, or insights in the comments section below. Your story can provide comfort and guidance to others navigating this challenging path, fostering a community of support and shared knowledge.

