Let’s address the central question immediately: “Adrenal fatigue” is not a recognized medical diagnosis.
Major medical bodies worldwide, including The Endocrine Society, do not support it as a legitimate condition due to a profound lack of scientific evidence.
The symptoms attributed to it, however—the deep exhaustion, brain fog and feeling of being perpetually overwhelmed—are undeniably real and can be debilitating.
You are not imagining your suffering. In fact, you are far from alone.
An estimated 3.3 million American adults live with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), a distinct and serious condition and countless others struggle with unexplained fatigue that significantly impairs their quality of life.
In this landscape of suffering, a simple, all-encompassing explanation like adrenal fatigue can feel like a lifeline. It offers a name for the invisible battle and a promise of a cure.
This article is for anyone who has felt dismissed by doctors or has desperately searched for answers online.
We will explore the origins of the adrenal fatigue theory, dissect the highest-quality scientific evidence, and clarify the critical differences between this unproven concept and real, diagnosable medical conditions.
Furthermore, we will analyze popular “cures” like the “adrenal cocktail” and provide an evidence-based roadmap to help you find the true cause of your symptoms and reclaim your vitality.
In This Article
What Is the Theory Behind Adrenal Fatigue?
To understand why the concept of adrenal fatigue is so compelling yet scientifically unsupported, we must first understand the theory itself.
This section explains the idea as its proponents present it, setting the stage for the critical analysis that follows.
Defining “Adrenal Fatigue”
So, what is adrenal fatigue according to its proponents?
The theory posits that our modern lives, filled with chronic stressors—from work deadlines and financial worries to emotional turmoil and poor diets—place an unrelenting demand on our adrenal glands.
These two small glands, which sit atop the kidneys, are central to our stress response.
The core idea is that this prolonged, excessive stress “overworks” or “burns out” the adrenal glands.
According to the theory, they eventually become “fatigued” and can no longer produce adequate levels of hormones, most notably cortisol.
This supposed state of low cortisol is then blamed for a wide array of non-specific symptoms, creating a condition that is said to be a milder, subclinical form of true adrenal failure.
Commonly Associated Symptoms
Proponents of the adrenal fatigue theory link it to a constellation of vague but distressing symptoms.
If you’ve researched this topic, you’ve likely encountered lists like this:
- Persistent, overwhelming fatigue: A deep tiredness that is not relieved by sleep.
- Difficulty waking up: Feeling groggy and “not a morning person”, often needing caffeine to get started.
- Sleep disturbances: Trouble falling asleep or staying asleep, despite being exhausted.
- Cravings for salty or sugary foods: An intense desire for specific types of food, believed to be the body’s attempt to compensate for electrolyte or energy imbalances.
- Body aches and muscle weakness: Unexplained soreness and a feeling of physical weakness.
- Brain fog: Difficulty concentrating, memory lapses and a feeling of mental cloudiness.
- Low mood and irritability: Symptoms that can overlap with depression or anxiety.
- Increased susceptibility to illness: A feeling that you’re always “coming down with something”.
- Low libido: A decreased interest in sex.
The appeal of the diagnosis is clear: it takes a collection of common, frustrating symptoms and organizes them under a single, plausible-sounding physiological cause.
The Origin of the Concept
The term “adrenal fatigue” is not new, but it was propelled into the public consciousness and alternative health mainstream by chiropractor and naturopath James Wilson.
His 2001 book, “Adrenal Fatigue: The 21st Century Stress Syndrome”, provided a name and a framework for people experiencing chronic stress and fatigue.
The book and the concept flourished outside the world of evidence-based medicine.
It gained traction in naturopathic, chiropractic, and functional medicine circles, promoted through websites, books and practitioners who offered diagnostic tests (like saliva cortisol panels) and proprietary supplement protocols.
It’s crucial to understand that this concept did not emerge from endocrinology research, rather, it was developed and popularized in a parallel system of alternative health.
The Role of the Adrenal Glands and Cortisol
To properly evaluate the adrenal fatigue theory, a basic understanding of the body’s stress-response system is essential.
This system is known as the Hypothalamic-Pituitary-Adrenal (HPA) axis.
- The Trigger (Hypothalamus): When your brain perceives a threat (physical or psychological), a region called the hypothalamus releases Corticotropin-Releasing Hormone (CRH).
- The Messenger (Pituitary Gland): CRH travels to the pituitary gland, which then releases Adrenocorticotropic Hormone (ACTH) into the bloodstream.
- The Action (Adrenal Glands): ACTH acts as a signal to your adrenal glands, telling them to produce and release a surge of hormones, most importantly, cortisol.
Cortisol is the body’s primary stress hormone. It increases blood sugar for quick energy, sharpens focus and temporarily dials down non-essential functions like digestion and the immune response—the classic “fight-or-flight” state.
In a healthy person, cortisol levels follow a natural daily rhythm (a diurnal rhythm): they are highest in the morning to help you wake up and gradually decline throughout the day, reaching their lowest point at night to allow for sleep.
The HPA axis has sophisticated feedback loops, when cortisol levels get high enough, they signal the hypothalamus and pituitary to stop releasing CRH and ACTH, thus turning off the stress response.
The adrenal fatigue theory hinges on the idea that this finely tuned system can be “broken” by chronic stress, leading to depleted cortisol. The next section will examine whether there is any scientific evidence to support this claim.
Key Points: The Theory of Adrenal Fatigue
- Core Idea: Chronic stress “burns out” the adrenal glands, causing low cortisol.
- Symptoms: It’s linked to a broad range of non-specific symptoms like fatigue, cravings and brain fog.
- Origin: Popularized by James Wilson’s 2001 book, it exists primarily in alternative medicine.
- Mechanism: It proposes a failure of the HPA axis, the body’s central stress-response system.
The Scientific Verdict: What the Evidence Actually Says
While the theory of adrenal fatigue sounds plausible, a medical concept’s validity is not determined by its plausibility but by rigorous scientific evidence.
In this section, we will move from theory to fact, examining the consensus of the medical community and the highest-quality research available.
The Overwhelming Medical Consensus
The position of the global endocrinology community is clear, consistent and unambiguous.
Major professional organizations that specialize in hormones and metabolism do not recognize adrenal fatigue as a real medical condition.
The Endocrine Society, the world’s leading organization for endocrinologists, states it plainly:
“No scientific proof exists to support adrenal fatigue as a true medical condition. Doctors are concerned that if you are told you have this condition, the real cause of your symptoms may not be found and treated correctly”.
This position is echoed by other prestigious medical institutions.
The Mayo Clinic refers to it as a “vague label” and notes, “there is no evidence to support this theory”.
Similarly, Harvard Medical School highlights the disconnect, stating, “The Endocrinologists are categorical: ‘no scientific proof exists to support adrenal fatigue as a true medical condition'”.
This is not a matter of debate within mainstream medicine. The consensus is built on a lack of credible, reproducible evidence that links the symptoms of fatigue to impaired adrenal gland function in the way the theory describes.
Dissecting the Landmark Systematic Review
The most definitive piece of evidence on this topic comes from a 2016 systematic review published in the peer-reviewed journal BMC Endocrine Disorders.
A systematic review is one of the highest forms of medical evidence because it collects and critically analyzes all relevant research on a specific question.
The study, titled “Adrenal fatigue does not exist: a systematic review“, set out to determine if there was any scientific substantiation for the condition.
The researchers searched major medical databases for all studies that assessed adrenal function (via cortisol testing) in fatigued individuals.
Methodology and Findings
Out of nearly 3.500 initial articles, the researchers identified 58 studies that met their quality criteria.
These studies used various methods to assess the HPA axis, including:
- Salivary Cortisol Rhythm (SCR): Measuring cortisol levels in saliva at multiple points throughout the day.
- Cortisol Awakening Response (CAR): Measuring the natural cortisol spike that occurs 30-45 minutes after waking.
- Direct Awakening Cortisol (DAC): Measuring cortisol right at the moment of waking.
If the adrenal fatigue theory were true, one would expect to see a consistent pattern of low or blunted cortisol levels in fatigued individuals compared to healthy controls.
The review found the exact opposite: the results were wildly inconsistent and contradictory.
- In studies measuring the full salivary cortisol rhythm, 61.5% found no difference between fatigued and healthy patients.
- In studies looking at the cortisol awakening response, results were split: 51.9% showed a normal response, 33.3% showed a diminished response, and 14.8% showed an increased response.
- The review also noted significant methodological flaws in many of the studies, including a lack of standardized testing methods and inconsistent definitions of “fatigue”.
The Unambiguous Conclusion
The authors of the systematic review did not mince words. They concluded:
“This systematic review proves that there is no substantiation that ‘adrenal fatigue’ is an actual medical condition. Therefore, adrenal fatigue is still a myth”.
They found no consistent evidence that fatigue was associated with impaired adrenal function.
The very tests that proponents use to “diagnose” the condition were shown to be unreliable and unable to differentiate fatigued people from healthy ones in a predictable way.
Visualizing the Inconsistency: Study Results on Cortisol and Fatigue
To make the findings of the 2016 systematic review more tangible, the chart below visualizes the conflicting results for the Cortisol Awakening Response (CAR), one of the most commonly studied markers.
If “adrenal fatigue” were a consistent physiological state of low cortisol, we would expect the vast majority of studies to find a “Diminished Response”.
Instead, the data is scattered, demonstrating a lack of a clear scientific signal.
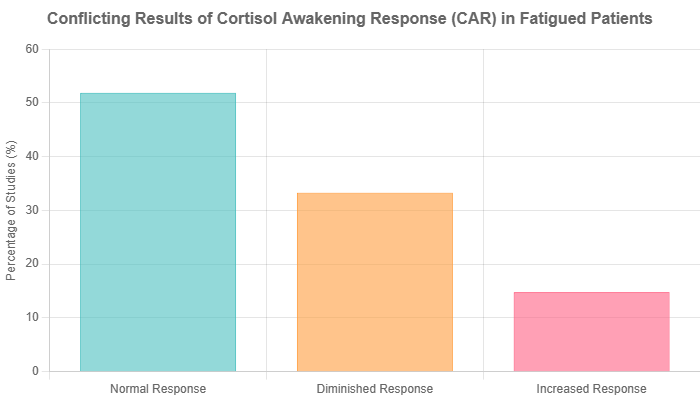
As the chart illustrates, over half of the studies found a completely normal cortisol response in fatigued individuals.
The lack of a consistent pattern is the primary reason why the scientific community rejects the adrenal fatigue hypothesis.
Why the “Adrenal Burnout” Theory is Physiologically Flawed
Beyond the lack of direct evidence, the core concept of the adrenal glands “fatiguing” or “burning out” is inconsistent with our understanding of physiology.
The adrenal glands are incredibly robust organs designed to respond to the body’s needs.
As Dr. Anat Ben-Shlomo, an endocrinologist at Cedars-Sinai, explains, “When you’re stressed, the adrenal glands actually produce more of the cortisol and other hormones you need. They will give you all that’s necessary”.
The body’s intricate HPA axis feedback loop is designed to regulate this process. The glands don’t simply run out of the ability to produce hormones from overuse, like a muscle tiring after exercise.
While extremely prolonged and severe chronic stress can lead to dysregulation of the HPA axis, this often manifests as inappropriately high cortisol levels or a disrupted diurnal rhythm, not a simple “depletion”.
The idea of the glands just giving up is a simplistic metaphor that doesn’t align with the complex reality of human endocrinology.
Key Points: The Scientific Verdict
- Medical Consensus: “Adrenal fatigue” is not a real medical diagnosis and is rejected by all major endocrinology and medical organizations.
- Highest-Quality Evidence: A major 2016 systematic review of 58 studies found no scientific basis to support the existence of adrenal fatigue.
- Inconsistent Data: Tests used to “diagnose” the condition show contradictory and unreliable results, failing to consistently differentiate fatigued from healthy individuals.
- Physiologically Flawed: The concept of adrenal glands “burning out” is a metaphor that does not align with the known function of the HPA axis, which tends to increase cortisol production under stress.
If Not Adrenal Fatigue, Then What? Real Medical Explanations for Your Symptoms
The most significant danger of the “adrenal fatigue” label is not just that it’s scientifically baseless, but that it can mask the true, underlying cause of a person’s suffering.
Your symptoms are real, and they deserve a real diagnosis. This section explores the legitimate medical conditions that can cause the very symptoms often misattributed to adrenal fatigue.
The Danger of a Misdiagnosis
When someone accepts “adrenal fatigue” as their diagnosis, they may delay or avoid seeking a proper medical evaluation.
This can have serious consequences. A treatable condition like hypothyroidism or sleep apnea could go undiagnosed for years, while the person spends time, money and emotional energy on unproven supplements and protocols.
Worse, the symptoms could be a sign of a more serious underlying illness. Accepting a pseudoscientific label can create a false sense of security, preventing a timely and potentially life-saving diagnosis.
The primary mission of a healthcare provider is to rule out these real conditions first.
Adrenal Insufficiency: A Real, Testable Condition
It is critically important to distinguish the myth of “adrenal fatigue” from the reality of Adrenal Insufficiency.
Adrenal Insufficiency is a real, often rare, but serious medical condition where the adrenal glands are damaged and cannot produce enough cortisol and, in some cases, aldosterone.
- Primary Adrenal Insufficiency (Addison’s Disease): This typically occurs when the immune system attacks the adrenal glands.
- Secondary Adrenal Insufficiency: This happens when the pituitary gland doesn’t produce enough ACTH, so the adrenal glands don’t receive the signal to make cortisol. This can be caused by tumors, surgery, or, ironically, the long-term use of steroid medications (like those sometimes found in “adrenal support” supplements).
Unlike the vague symptoms of “adrenal fatigue”, Adrenal Insufficiency has more specific signs and is diagnosed with validated, standardized medical tests.
Symptoms of Adrenal Insufficiency Include:
- Chronic, worsening fatigue
- Muscle weakness
- Loss of appetite and unintentional weight loss
- Low blood pressure (hypotension), which can cause dizziness upon standing
- Nausea, vomiting and abdominal pain
- Darkening of the skin (hyperpigmentation), especially in skin creases, scars, and on the gums (in Addison’s disease)
- Salt craving
Diagnosis: An endocrinologist diagnoses this condition using blood tests that measure baseline cortisol levels and, most definitively, an ACTH stimulation test. In this test, a synthetic version of ACTH is injected, and blood cortisol levels are measured. If the adrenal glands are damaged, they will fail to respond and produce cortisol, confirming the diagnosis.
Comparative Table: “Adrenal Fatigue” vs. Real Medical Conditions
To provide maximum clarity, this table compares the key features of the “adrenal fatigue” theory against two recognized medical conditions: Adrenal Insufficiency and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
| Feature | “Adrenal Fatigue” (Theory) | Adrenal Insufficiency (Medical Condition) | ME/CFS (Medical Condition) |
|---|---|---|---|
| Medical Recognition | Not recognized by any major medical or endocrinology society. | Recognized as a rare but serious endocrine disorder. | Recognized as a complex, multi-system neuroimmune illness. |
| Key Cause | Theory: Adrenal glands “burn out” from chronic stress. | Fact: Adrenal gland damage (e.g., autoimmune) or pituitary dysfunction. | Fact: Exact cause is unknown, but involves immune dysregulation, cellular energy metabolism issues and often follows an infection. |
| Primary Symptoms | Vague: Fatigue, cravings, brain fog, body aches. | Specific: Fatigue plus weight loss, low blood pressure, skin darkening, vomiting. | Specific: Severe fatigue plus post-exertional malaise (PEM), unrefreshing sleep, cognitive impairment, and/or orthostatic intolerance. |
| Diagnostic Method | Unproven methods like saliva tests or questionnaires. No standardized criteria. | Validated blood tests, primarily the ACTH stimulation test. | Clinical diagnosis based on strict criteria after ruling out other conditions. No single biomarker test exists yet. |
Other Potential Culprits for Fatigue
Your persistent fatigue is a valid signal that something is wrong.
If it’s not “adrenal fatigue”, what could it be? A thorough medical evaluation can uncover a wide range of potential causes. Here are some of the most common:
Hypothyroidism
The thyroid gland, located in your neck, produces hormones that regulate your metabolism.
When it’s underactive (hypothyroidism), your entire body slows down.
Symptoms include fatigue, weight gain, feeling cold, dry skin, constipation and brain fog.
It is easily diagnosed with a simple blood test (TSH and Free T4) and treated with thyroid hormone replacement medication.
Sleep Apnea
Obstructive sleep apnea is a condition where you repeatedly stop and start breathing for brief periods during sleep.
These episodes can happen hundreds of times a night, preventing you from reaching deep, restorative sleep.
The hallmark symptom is severe daytime sleepiness, even after a full night in bed.
Other signs include loud snoring, waking up gasping for air, and morning headaches.
It is diagnosed with a sleep study and treated effectively with devices like a CPAP machine.
Depression and Anxiety
Mental health conditions are physical health conditions. The neurochemical changes associated with depression can cause profound fatigue, lack of motivation and sleep disturbances.
Anxiety can be mentally and physically exhausting, keeping the body in a constant state of high alert.
These conditions are not a sign of weakness and can be effectively managed with therapy, medication and lifestyle changes.
Anemia (Iron Deficiency)
Iron is a critical component of hemoglobin, the protein in red blood cells that carries oxygen to your tissues.
When you are deficient in iron, your body can’t get the oxygen it needs, leading to profound fatigue, weakness, shortness of breath and pale skin.
It is particularly common in menstruating women. A simple blood test (CBC and ferritin) can diagnose it and treatment involves iron supplementation and dietary changes.
Fibromyalgia
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues.
It’s believed to be caused by the way the brain and spinal cord process pain signals.
While there is no single cure, its symptoms can be managed with a combination of medication, exercise and stress-reduction techniques.
Autoimmune Diseases
In autoimmune conditions like Lupus or Rheumatoid Arthritis, the immune system mistakenly attacks the body’s own tissues.
This chronic inflammation is incredibly draining and is a common cause of severe fatigue, in addition to other system-specific symptoms like joint pain or skin rashes.
Diagnosis involves specific blood tests and clinical evaluation.
Deconstructing Popular “Cures”: The Adrenal Cocktail and Supplements
Where a pseudoscientific diagnosis exists, a market for “cures” is sure to follow.
The adrenal fatigue niche is a multi-million dollar industry built on selling hope in the form of supplements and special drinks.
This section critically examines the most popular of these “remedies”.
The Rise of the “Adrenal Cocktail”
A recent trend sweeping social media platforms like TikTok and Instagram is the “adrenal cocktail” (sometimes called a “cortisol cocktail”).
While recipes vary, the basic formula usually involves a mix of:
- Orange Juice (for Vitamin C)
- Coconut Water (for potassium)
- A pinch of Sea Salt (for sodium and trace minerals)
The theory promoted alongside the drink is that these specific nutrients are essential for adrenal gland function and help “replenish” them.
Vitamin C is indeed stored in high concentrations in the adrenal glands, and sodium and potassium are key electrolytes involved in adrenal hormone function.
The Scientific Take
Is there anything wrong with this drink? For most healthy people, no.
It’s a hydrating beverage that provides some vitamins and electrolytes. However, the claims made about it are unsubstantiated.
- It treats a non-existent condition: Since there is no evidence that the adrenal glands “fatigue”, there is no basis for the claim that this drink can “heal” or “support” them in the way described.
- Nutrient levels are not therapeutic: While the ingredients contain the target nutrients, the amounts are generally small and easily obtained from a balanced diet. Most people are not deficient in these specific nutrients to a degree that would cause severe fatigue.
- It doesn’t address the root cause: If your fatigue is caused by sleep apnea, anemia, or hypothyroidism, drinking an adrenal cocktail will do absolutely nothing to fix the underlying problem.
The adrenal cocktail is a classic example of a “health hack” that combines a plausible-sounding theory with a simple recipe, but it lacks any scientific evidence of efficacy for its stated purpose.
The Risks of “Adrenal Support” Supplements
Far more concerning than a harmless drink are the over-the-counter “adrenal support” supplements sold online and by some alternative practitioners.
These products pose significant risks for two main reasons.
1. Lack of Regulation
The dietary supplement industry in the United States is not regulated by the Food and Drug Administration (FDA) in the same way as prescription drugs. This means:
- Purity is not guaranteed: The bottle may contain contaminants or different ingredients than what is listed on the label.
- Potency is not guaranteed: The dose of the active ingredient can vary wildly from what is stated.
- Efficacy is not required: Manufacturers do not have to prove their product actually works before selling it.
2. Hidden and Dangerous Ingredients
The most alarming risk is that some of these “adrenal support” formulas have been found to contain undisclosed active ingredients, including actual steroid hormones (like hydrocortisone, a synthetic cortisol) or glandular extracts from animal adrenal glands.
Taking these potent substances without a medical diagnosis and prescription is incredibly dangerous.
If you take steroids when your body doesn’t need them, it can suppress your own HPA axis. Your pituitary gland stops sending the signal (ACTH) to your adrenals and they go dormant.
If you then suddenly stop taking the supplement, your body is left with no way to produce its own cortisol, potentially leading to a life-threatening adrenal crisis.
In a cruel irony, attempting to treat a fake disease can end up causing a real one: secondary adrenal insufficiency.
The Placebo Effect and Confounding Lifestyle Changes
Many people genuinely report feeling better after starting an “adrenal fatigue” protocol.
How can this be if the condition and the supplements are fake? The answer usually lies in two powerful factors.
First is the placebo effect. The act of taking control of one’s health, believing in a treatment, and receiving care from a practitioner can create powerful expectations that lead to real, perceived improvements in symptoms.
Second, and more importantly, these protocols almost always include positive lifestyle advice alongside the supplements.
They typically recommend reducing stress, improving diet, cutting out processed foods and sugar, prioritizing sleep and engaging in gentle exercise.
These are all evidence-based strategies that are known to improve energy levels and well-being, regardless of the underlying cause.
The person feels better because of the lifestyle changes, but mistakenly attributes the improvement to the expensive, unproven supplements they were sold.
An Evidence-Based Action Plan for Wellness
If you’re struggling with the symptoms commonly associated with “adrenal fatigue”, the goal is not to “heal your adrenals” but to identify and address the true root cause of your suffering.
This requires abandoning the myth and embracing an evidence-based, systematic approach to your health.
Step 1: Get a Proper Medical Diagnosis
This is the single most important step. Stop self-diagnosing and self-treating.
Schedule a comprehensive appointment with a primary care physician or an endocrinologist.
- Be specific about your symptoms: Keep a journal for a few weeks before your appointment. Track your fatigue levels (on a scale of 1-10), sleep patterns, food cravings, mood and any other symptoms.
- Advocate for yourself: Clearly state your symptoms and their impact on your life. Say, “I am experiencing debilitating fatigue that is not relieved by sleep, and I want to investigate the potential medical causes”.
- Request specific tests: Based on your symptoms, ask your doctor to consider testing for the common culprits: a complete blood count (for anemia), a full thyroid panel (TSH, Free T4), vitamin deficiencies (B12, Vitamin D) and inflammatory markers.
Do not accept “adrenal fatigue” as a diagnosis from any practitioner. Insist on investigating recognized medical conditions until you have a clear answer or have ruled out the major possibilities.
Step 2: Prioritize Foundational Sleep Hygiene
No supplement or diet can fix a chronic sleep deficit. Improving sleep is non-negotiable for restoring energy.
- Maintain a Consistent Schedule: Go to bed and wake up at the same time every day, even on weekends. This stabilizes your body’s internal clock (circadian rhythm).
- Create a Dark, Cool, Quiet Sanctuary: Your bedroom should be optimized for sleep. Use blackout curtains, a white noise machine and set the thermostat to a cool temperature.
- Implement a Digital Sunset: Stop using all screens (phones, tablets, TVs, computers) at least 60-90 minutes before bed. The blue light they emit suppresses melatonin, the hormone that makes you sleepy.
- Avoid Stimulants and Alcohol Before Bed: Stop consuming caffeine by early afternoon. While alcohol may make you feel drowsy initially, it disrupts sleep architecture later in the night.
Step 3: Implement Evidence-Based Stress Management
While stress doesn’t cause “adrenal fatigue”, it absolutely causes real, physiological changes that can lead to exhaustion and illness. Managing your stress response is key.
- Mindfulness and Meditation: Apps like Calm or Headspace can guide you through daily practices that have been scientifically shown to lower cortisol and reduce the brain’s reactivity to stress.
- Gentle Movement: High-intensity exercise can be an additional stressor when you’re already depleted. Focus on restorative activities like walking in nature, yoga or tai chi.
- Deep Breathing Exercises: Simple techniques like box breathing (inhale for 4 seconds, hold for 4, exhale for 4, hold for 4) can instantly activate the parasympathetic nervous system, your body’s “rest and digest” mode.
Step 4: Adopt a Balanced, Nutrient-Dense Diet
Forget unproven “cocktails” and focus on the fundamentals of a diet that supports stable energy.
- Stabilize Blood Sugar: Avoid sugary snacks and refined carbohydrates that cause energy spikes and crashes. At each meal, combine a source of protein, healthy fat and high-fiber carbohydrates (like vegetables and whole grains).
- Focus on Whole Foods: Build your diet around foods in their most natural state: fruits, vegetables, lean proteins, nuts, seeds and legumes. These are packed with the vitamins and minerals your body actually needs.
- Hydrate with Water: Dehydration is a common and often overlooked cause of fatigue. Aim to drink water consistently throughout the day.
Step 5: Re-evaluate Your Relationship with Stimulants
When you’re exhausted, it’s natural to reach for caffeine to get through the day.
However, this can create a vicious cycle. Over-reliance on stimulants can mask the severity of your fatigue, disrupt your natural sleep-wake cycle, and lead to an inevitable crash.
Consider gradually reducing your caffeine intake or limiting it to the early morning.
This can help reset your body’s natural cortisol rhythm and give you a clearer picture of your baseline energy levels, which is valuable information for you and your doctor.
Frequently Asked Questions (FAQ)
1. Is adrenal fatigue a real medical diagnosis?
No, adrenal fatigue is not a real medical diagnosis recognized by endocrinologists or major medical organizations. It is a theory that lacks scientific support and is considered a myth by the mainstream medical community.
2. What’s the difference between adrenal fatigue and adrenal insufficiency?
Adrenal insufficiency is a real, rare medical condition where the adrenal glands don’t produce enough hormones, diagnosed by specific blood tests. “Adrenal fatigue” is an unproven theory that claims chronic stress exhausts the glands.
3. Can a saliva test diagnose adrenal fatigue?
No. While some alternative practitioners use them, salivary cortisol tests are not considered a reliable or validated method for diagnosing any form of adrenal dysfunction. A landmark systematic review found their results to be inconsistent and contradictory.
4. Does the “adrenal cocktail” work?
There is no scientific evidence that the “adrenal cocktail” can treat adrenal fatigue or any other medical condition. While its ingredients provide hydration and some nutrients, it does not “heal” the adrenal glands as claimed.
5. Are adrenal support supplements safe?
They can be very risky. They are not regulated by the FDA and may contain unknown ingredients or even hidden steroids that can suppress your body’s natural adrenal function, potentially causing actual adrenal insufficiency.
6. If my doctor says I don’t have adrenal fatigue, what should I do?
Work with your doctor to investigate other potential causes for your symptoms. Ask for tests to rule out recognized medical conditions like hypothyroidism, sleep apnea, anemia, vitamin deficiencies or depression.
7. Why do I feel so tired all the time?
Chronic fatigue can have many legitimate causes, including poor sleep quality, chronic psychological stress, nutritional deficiencies, and a wide range of underlying medical conditions. It is essential to get a comprehensive medical evaluation to find the true cause.
8. Who invented the term adrenal fatigue?
The term was popularized by chiropractor and naturopath James Wilson in his 2001 book, “Adrenal Fatigue: The 21st Century Stress Syndrome”. The concept is not accepted in the field of evidence-based medicine or endocrinology.
Conclusion
The journey through chronic, unexplained fatigue is frustrating and isolating. In that vulnerability, the concept of “adrenal fatigue” offers a simple narrative and a clear enemy.
However, the overwhelming weight of scientific evidence shows that this narrative is a myth.
The adrenal glands do not “fatigue” from stress, and the tests and treatments promoted for this non-existent condition are unproven and potentially dangerous.
The most important takeaway is this: while adrenal fatigue is not real, your symptoms are.
Your exhaustion is real. Your brain fog is real. Your suffering is real, and it deserves to be taken seriously.
The true danger of the “adrenal fatigue” label is that it acts as a roadblock to genuine healing.
It distracts from the critical work of uncovering the real, treatable medical conditions that are often the true culprits behind the symptoms. By clinging to a myth, you may be delaying a diagnosis that could change your life.
The path to reclaiming your energy begins with letting go of this pseudoscientific dead end.
We encourage you to stop self-diagnosing and partner with a qualified healthcare professional.
Empower yourself with knowledge, advocate for a thorough investigation, and commit to the evidence-based lifestyle strategies that are proven to build resilience and well-being.
Your path to relief is not in a supplement bottle or a trendy cocktail, but in the diligent and compassionate search for a real diagnosis and a personalized, scientific plan for your health.
Have you struggled with unexplained fatigue? Have you been given an “adrenal fatigue” diagnosis? Share your experience or your journey to finding a real diagnosis in the comments below to help others who are on a similar path.

