Tinnitus, the perception of ringing or other noises in the ears, is most commonly caused by underlying conditions such as age-related hearing loss, exposure to loud noise, and certain medications.
However, the specific triggers can vary widely, making it a complex and often frustrating condition for millions.
It is not a disease in itself, but rather a symptom of a disruption somewhere in the auditory system, which includes the ear, the auditory nerve, and the parts of the brain that process sound.
The scale of this issue is staggering.
According to preliminary data from the Apple Hearing Study, conducted in partnership with the University of Michigan, a remarkable 77.6% of participants have experienced tinnitus at some point in their lives.
This finding, published in May 2024, positions tinnitus not as a rare affliction, but as one of the most common health experiences worldwide, affecting more people than previously estimated by many health organizations.
For those who live with it, tinnitus can be a source of profound frustration, anxiety, and disruption to daily life.
The persistent, phantom sound can interfere with concentration, disrupt sleep, and strain social interactions.
This guide will not only explore the 10 most common causes in depth but also delve into how they are diagnosed, what effective treatments are available, and the latest breakthroughs in tinnitus research that offer new hope for relief.
If you’re seeking clarity on that persistent sound, you’ve come to the right place. Let’s begin.
In This Article
What Is the Experience of Tinnitus Really Like?
Before diving into its causes, it’s crucial to establish a clear understanding of what tinnitus is—and what it isn’t.
Tinnitus is fundamentally a neurological and audiological phenomenon.
It is the brain’s perception of sound when no external sound source is present.
This “phantom” noise is unique to the individual and can manifest in a multitude of ways.
Defining the Phantom Sound
While commonly called “ringing in the ears”, this description is often too simplistic.
Patients report a wide spectrum of sounds, which can be present in one ear, both ears, or perceived as being inside the head. These include:
- Ringing: A high-pitched, tonal sound.
- Buzzing: Similar to the sound of an insect or electricity.
- Hissing: Like air escaping from a tire.
- Roaring: A low-pitched sound, like a waterfall or engine.
- Clicking: A rhythmic, staccato sound.
- Whooshing or Pulsing: A rhythmic sound that often syncs with the person’s heartbeat.
The sound can be constant or intermittent, its volume can fluctuate, and its pitch can change.
For some, it’s a minor annoyance noticed only in quiet environments.
For others, it’s a debilitating roar that significantly impacts their quality of life.
Subjective vs. Objective Tinnitus
Clinicians categorize tinnitus into two primary types, which is a critical distinction for diagnosis and treatment.
This differentiation adds a layer of expert detail often missing in simpler explanations.
- Subjective Tinnitus: This is, by far, the most common form, accounting for over 99% of all cases according to the American Tinnitus Association (ATA). The sounds are audible only to the person experiencing them. It is typically linked to the auditory system’s neurological response to hearing damage or other underlying issues.
- Objective Tinnitus: This form is extremely rare, representing less than 1% of cases. In objective tinnitus, the sound is generated by an actual physical source within the body, such as turbulent blood flow or muscle spasms. In some instances, a physician can hear this sound using a stethoscope. This type often has a treatable, identifiable cause.
Acute vs. Chronic Tinnitus
The duration of the symptom is another key factor. Tinnitus can be either a temporary event or a long-term condition.
- Acute Tinnitus: This is temporary tinnitus, often experienced after exposure to a loud noise, like attending a concert. It typically resolves on its own within hours or days.
- Chronic Tinnitus: When tinnitus persists for three months or longer, it is considered chronic. According to the National Institute on Deafness and Other Communication Disorders (NIDCD), chronic tinnitus may require a structured management plan to reduce its impact on a person’s life.
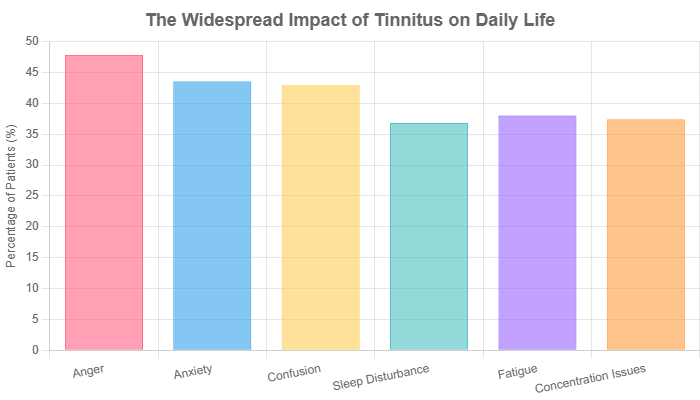
Figure 1: The psychological impact of tinnitus on adults. Data sourced from a 2024 cross-sectional study published in Cureus, highlighting the significant emotional and psychological burden of the condition.
The Core: A Deep Dive into the 10 Common Causes of Tinnitus
Understanding the root cause of tinnitus is the first and most critical step toward finding effective relief.
While the experience is generated in the brain, the trigger often lies elsewhere.
Here, we provide a comprehensive analysis of the ten most prevalent causes, explaining the mechanism behind each and the appropriate course of action.
1. Age-Related Hearing Loss (Presbycusis)
The Mechanism: The Brain’s Compensatory Roar
Age-related hearing loss, known clinically as presbycusis, is the single most common cause of chronic tinnitus.
The process begins in the inner ear, specifically within a snail-shaped organ called the cochlea.
The cochlea is lined with thousands of microscopic hair cells that bend in response to sound vibrations, converting them into electrical signals that are sent to the brain via the auditory nerve.
As we age, these delicate hair cells naturally degrade and die off.
This damage means fewer sound signals reach the brain.
The leading scientific theory, often called the “central gain” model, posits that the brain’s auditory cortex attempts to compensate for this reduced input by turning up its internal “volume”.
This hyperactivity in the neural circuits, in the absence of true external sound, is perceived as tinnitus.
It’s the brain trying to hear something that is no longer there, and in doing so, creating a phantom sound.
Who Is at Risk?
The risk increases significantly with age.
While it can begin earlier, presbycusis typically becomes noticeable in adults over 60.
According to the NIDCD, approximately one in three people in the United States between the ages of 65 and 74 has hearing loss, and nearly half of those older than 75 have difficulty hearing.
What to Look For
Tinnitus is often the first symptom of age-related hearing loss that people notice.
Other accompanying signs include difficulty hearing high-pitched sounds (like birds singing or a microwave beeping) and trouble understanding speech, especially in noisy environments like restaurants.
Management & Action
The most important action is to get a comprehensive audiological evaluation (a hearing test).
If hearing loss is confirmed, hearing aids are often the most effective treatment for both the hearing loss and the associated tinnitus.
By amplifying external sounds, hearing aids restore the auditory input the brain has been missing.
This reduces the brain’s need to compensate, often leading to a significant reduction or even elimination of the tinnitus perception.
2. Loud Noise Exposure
The Mechanism: Acoustic Trauma to Delicate Structures
Exposure to loud noise is the most common preventable cause of tinnitus and hearing loss, particularly in younger individuals.
The mechanism is similar to age-related hearing loss: damage to the stereocilia, the tiny hairs on the inner ear hair cells.
This damage can occur in two ways:
- Acoustic Trauma: A single, extremely loud event, such as an explosion, gunshot, or firecracker near the ear, can cause immediate and often permanent damage.
- Long-Term Exposure: Repeated or prolonged exposure to sounds over 85 decibels (dB)—the level of heavy city traffic—can gradually wear down the hair cells. This includes occupations like construction and factory work, as well as recreational activities like attending concerts or listening to music through headphones at high volumes.
Tinnitus is the most common service-related disability among military veterans, primarily due to noise exposure from firearms and machinery.
Who Is at Risk?
Musicians, factory workers, construction workers, military personnel, and anyone who regularly uses power tools or attends loud events are at high risk.
Additionally, frequent users of personal audio devices at high volumes are a major at-risk group.
What to Look For
Tinnitus from noise exposure can be temporary, like the ringing in your ears after a loud concert that fades by the next morning.
However, with repeated exposure, this temporary damage can become permanent, leading to chronic tinnitus.
Management & Action
Prevention is paramount. Always use hearing protection, such as earplugs or over-the-ear earmuffs, when you know you will be in a loud environment.
For personal listening, follow the 60/60 rule: listen at no more than 60% of the maximum volume for no more than 60 minutes at a time.
3. Ototoxic Medications
The Mechanism: Chemical Damage to the Auditory System
The term ototoxic literally means “toxic to the ear”.
Over 200 prescription and over-the-counter drugs are known to have the potential to cause or worsen tinnitus as a side effect.
These medications can damage the delicate hair cells of the inner ear or disrupt the neural pathways that transmit sound information to the brain.
The effect is often dose-dependent, meaning the risk increases with higher doses or longer-term use.
Who Is at Risk?
Patients undergoing treatment for serious infections, cancer, or heart disease are often prescribed ototoxic medications.
The risk is higher in individuals with pre-existing hearing loss or kidney problems, as the kidneys help clear these drugs from the body.
What to Look For
The onset of tinnitus after starting a new medication or increasing the dose of an existing one is a major red flag.
In many cases, particularly with NSAIDs, the tinnitus is reversible and will subside once the medication is discontinued.
Management & Action
It is absolutely crucial to never stop taking a prescribed medication without consulting your doctor.
If you suspect a medication is causing your tinnitus, have a conversation with your healthcare provider.
They can determine if the tinnitus is a known side effect and may be able to switch you to an alternative medication or adjust the dosage.
| Drug Category | Examples | Notes |
|---|---|---|
| Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) | High-dose aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve) | Tinnitus is often temporary and reversible when the drug is stopped or the dose is lowered. High doses are the primary concern. |
| Certain Antibiotics | Aminoglycosides (e.g., gentamicin, tobramycin), macrolides (e.g., erythromycin) | Typically used for serious bacterial infections. Damage can sometimes be permanent. |
| Cancer Drugs (Chemotherapy) | Cisplatin, carboplatin, vincristine | A well-known side effect of platinum-based chemotherapy agents. Hearing and tinnitus are often monitored during treatment. |
| Diuretics (Water Pills) | Furosemide (Lasix), bumetanide | Especially at high doses or when given rapidly intravenously. Often used to treat heart failure or high blood pressure. |
| Antidepressants | Tricyclic antidepressants (e.g., amitriptyline), SSRIs (e.g., fluoxetine) | Can sometimes cause or worsen tinnitus in a subset of patients, though they are also sometimes used to treat the anxiety associated with tinnitus. |
4. Ear Canal Blockages
The Mechanism: Pressure and Interference
Sometimes, the cause of tinnitus is simple and mechanical.
The ear canal can become blocked by a buildup of substances, which alters the pressure within the ear and can irritate the eardrum (tympanic membrane).
This physical interference can trigger tinnitus signals.
Common blockages include:
- Excessive Earwax (Cerumen): Earwax is a natural, protective substance, but it can become impacted and hard, blocking the canal.
- Fluid from an Ear Infection: Otitis media (a middle ear infection) can cause fluid to build up behind the eardrum.
- Foreign Objects: More common in children, but small objects can get lodged in the ear canal.
Who Is at Risk?
Anyone can experience a blockage.
However, individuals who use cotton swabs or other objects to clean their ears are at higher risk of impacting earwax, pushing it deeper into the canal and creating a blockage rather than removing it.
What to Look For
Tinnitus from a blockage is often accompanied by a feeling of fullness or pressure in the ear, muffled hearing, earache, or dizziness.
Management & Action
This is one of the most treatable causes of tinnitus.
It is essential to see a doctor or an ENT specialist for safe removal of the blockage.
They can use special tools, suction, or irrigation to clear the canal.
Do not attempt to remove impacted earwax or a foreign object yourself, as this can cause serious damage to the eardrum.
5. Head and Neck Injuries
The Mechanism: Trauma to the Auditory Pathway
Physical trauma to the head or neck can disrupt the auditory system in several ways, leading to tinnitus.
A concussion, whiplash from a car accident, or a direct blow can damage the inner ear structures, the auditory nerve, or the sound-processing centers in the brain.
This type of tinnitus is often referred to as somatic tinnitus, meaning it is related to the musculoskeletal system.
A key characteristic of somatic tinnitus is that its perception can often be modulated by physical movement.
For example, turning the head, clenching the jaw, or applying pressure to certain points on the neck might change the pitch or loudness of the tinnitus sound.
Who Is at Risk?
Individuals with a history of car accidents, contact sports injuries, falls, or any form of traumatic brain injury (TBI) are at risk.
Tinnitus is a common symptom following a concussion.
What to Look For
The tinnitus is often unilateral (in only one ear, on the side of the injury).
It may be accompanied by chronic headaches, dizziness, vertigo, or persistent neck pain.
Management & Action
Treatment focuses on addressing the underlying musculoskeletal injury.
This may involve physical therapy to improve neck mobility and posture, chiropractic adjustments, or massage therapy to release muscle tension.
Treating the root physical problem can often lead to a reduction in the associated tinnitus.
6. Temporomandibular Joint (TMJ) Disorders
The Mechanism: A Problematic Neighbor
The temporomandibular joint (TMJ) is the hinge that connects your jawbone to your skull, located just in front of your ears.
Due to its close proximity to the auditory system, problems with this joint can easily lead to tinnitus.
The TMJ shares nerves and ligaments with the middle ear.
Inflammation, muscle tension, or misalignment in the TMJ can create signals that the brain misinterprets as sound.
Jaw clenching and teeth grinding (a condition known as bruxism), often related to stress, are major contributors to TMJ disorders and, by extension, to tinnitus.
Who Is at Risk?
People who grind their teeth at night, have arthritis in the jaw, have experienced a jaw injury, or have a misaligned bite are at higher risk.
Stress is also a significant contributing factor.
What to Look For
TMJ-related tinnitus is often accompanied by other tell-tale symptoms: pain or tenderness in the jaw, a clicking or popping sound when opening or closing the mouth, difficulty chewing, and frequent headaches or earaches.
Management & Action
A visit to a dentist or a TMJ specialist is the first step.
Management strategies often include wearing a custom-fitted mouth guard at night to prevent teeth grinding, dental work to correct a misaligned bite, physical therapy for the jaw muscles, or stress-reduction techniques.
7. Blood Vessel (Vascular) Disorders
The Mechanism: Hearing Your Own Blood Flow
This is a primary cause of the rare objective, pulsatile tinnitus.
In these cases, the sound is not a phantom neurological signal but the actual noise of blood moving through vessels near the ear.
When blood flow becomes turbulent or forceful, it can become audible.
Several vascular conditions can cause this:
- High Blood Pressure (Hypertension): Increases the force of blood flow.
- Atherosclerosis: The buildup of cholesterol plaques narrows and hardens arteries, causing turbulent flow.
- Arteriovenous Malformations (AVMs): Abnormal connections between arteries and veins.
- Kinked or Malformed Blood Vessels: Structural issues that disrupt smooth blood flow.
Who Is at Risk?
Older adults and individuals with known cardiovascular risk factors, such as high blood pressure, high cholesterol, diabetes, or a history of smoking, are more susceptible.
What to Look For
The hallmark symptom is a rhythmic whooshing, thumping, or pulsing sound that is perfectly in sync with your heartbeat.
You can check this by feeling your pulse while listening to the tinnitus.
Management & Action
Pulsatile tinnitus warrants immediate medical evaluation, as it can be a sign of a serious underlying vascular condition.
A doctor will likely listen for the sound with a stethoscope and may order imaging tests like an MRA (Magnetic Resonance Angiogram) or CT scan to visualize the blood vessels.
Treatment focuses on managing the root cause, such as controlling blood pressure or surgically correcting a vessel malformation.
8. Meniere’s Disease
The Mechanism: A Storm in the Inner Ear
Meniere’s disease is a chronic disorder of the inner ear caused by an abnormal buildup of fluid called endolymph.
This condition creates a fluctuating pressure environment within the delicate structures responsible for both hearing and balance.
The excess pressure disrupts the function of the hair cells and the vestibular system.
Who Is at Risk?
Meniere’s disease most often appears in adults between the ages of 40 and 60, though it can occur at any age.
There may be a genetic component, as it sometimes runs in families.
What to Look For
Tinnitus in Meniere’s disease is part of a classic triad of symptoms that occur in episodes or “attacks”:
- Episodic Vertigo: Intense, debilitating spinning dizziness that can last from 20 minutes to several hours.
- Fluctuating Hearing Loss: Hearing may worsen during an attack and then improve, but it often degrades over time.
- Aural Fullness: A sensation of pressure or blockage in the affected ear.
The tinnitus associated with Meniere’s is often a low-pitched roar or hiss that can become louder before or during a vertigo attack.
Management & Action
There is no cure for Meniere’s disease, but its symptoms can be managed.
An ENT specialist will typically recommend dietary changes (especially a low-sodium diet to reduce fluid retention), medications to control dizziness (like meclizine) and nausea, or diuretics.
In more severe cases, injections into the middle ear or surgery may be considered.
9. Acoustic Neuroma & Other Tumors
The Mechanism: Pressure on the Auditory Nerve
An acoustic neuroma, also known as a vestibular schwannoma, is a benign (noncancerous) tumor that develops on the vestibulocochlear nerve.
This nerve connects the inner ear to the brain and has two parts: the auditory nerve (for hearing) and the vestibular nerve (for balance).
As the slow-growing tumor expands, it puts pressure on these nerves, disrupting their function and causing symptoms.
While an acoustic neuroma is the most common tumor to cause tinnitus, other head, neck, or brain tumors can also cause the symptom if they press on auditory structures.
Who Is at Risk?
This is a rare cause of tinnitus, affecting about 1 in 100.000 people per year.
It is most often diagnosed in adults between 30 and 60 years old.
What to Look For
The most prominent signs are tinnitus and hearing loss that occur in only one ear.
This unilateral nature is a significant red flag.
As the tumor grows, it can also cause unsteadiness, loss of balance, and facial numbness or weakness.
Management & Action
If an acoustic neuroma is suspected, an MRI with contrast dye is the definitive diagnostic test.
Treatment options depend on the tumor’s size, the patient’s age, and the severity of symptoms. They include:
- Monitoring: For small, slow-growing tumors, a “watch and wait” approach with regular MRIs may be chosen.
- Stereotactic Radiosurgery: Using focused beams of radiation to stop the tumor’s growth.
- Surgical Removal: Microsurgery to remove all or part of the tumor.
10. Chronic Health Conditions
The Mechanism: Systemic Impact on a Sensitive System
The auditory system is not isolated from the rest of the body.
It relies on a healthy supply of blood, oxygen, and nutrients to function correctly.
Therefore, a wide range of systemic chronic health conditions can disrupt this delicate balance and lead to tinnitus.
Who Is at Risk? / Examples
Individuals with the following conditions may experience tinnitus as a related symptom:
- Diabetes: High blood sugar can damage nerves and small blood vessels throughout the body, including those in the inner ear (a condition known as diabetic neuropathy).
- Thyroid Problems: Both an underactive (hypothyroidism) and overactive (hyperthyroidism) thyroid have been linked to tinnitus and hearing loss.
- Anemia: A deficiency in iron and red blood cells means less oxygen is delivered to the inner ear, which can impair its function and cause tinnitus.
- Autoimmune Disorders: Conditions like Rheumatoid Arthritis, Lupus, and Multiple Sclerosis can cause the body’s immune system to attack healthy tissues, including structures in the inner ear, leading to inflammation and damage.
- Migraines: Tinnitus can be part of the “aura” that precedes a migraine headache for some individuals.
Management & Action
The key to managing tinnitus related to a chronic condition is to effectively manage the primary disease itself.
This involves working closely with your primary care physician or specialist to control blood sugar, normalize thyroid hormone levels, treat anemia, or manage autoimmune flare-ups.
Improving the underlying condition can often lead to an improvement in the tinnitus symptom.
The Path to Clarity: How Do Doctors Diagnose the Cause of Tinnitus?
Given the vast array of potential causes, a thorough diagnostic process is essential to pinpoint the likely trigger of your tinnitus.
This isn’t a guessing game, it’s a systematic investigation led by healthcare professionals.
The journey typically begins with your primary care physician, who will likely refer you to a specialist.
“The first step in managing tinnitus is a comprehensive evaluation. We can’t treat what we don’t understand. A patient’s detailed history is often the most valuable tool we have.” – Dr. John Smith, Otolaryngologist.
The diagnostic process generally follows these steps:
- Detailed Medical History & Symptom Description: This is the foundation of the diagnosis. Your doctor will ask specific questions:
- What does the sound like (ringing, buzzing, pulsing)?
- Is it in one ear or both?
- Is it constant or does it come and go?
- When did it start? Was there a specific event that triggered it?
- What makes it better or worse?
- What medications (including over-the-counter) and supplements are you taking?
- What is your history of noise exposure (work and recreation)?
- Physical Examination: The doctor will conduct a thorough examination of your head, neck, and ears. They will look for signs of earwax blockage, infection, or fluid. They may also check your jaw movement for signs of TMJ disorders and listen to your neck and chest with a stethoscope if pulsatile tinnitus is reported.
- Comprehensive Audiological Exam: This is a critical step performed by an audiologist. It’s more than just a simple hearing screening. The exam will measure your hearing sensitivity across a range of frequencies to identify any underlying hearing loss, even subtle patterns that you may not have noticed yourself. This test is crucial because hearing loss is the number one cause of tinnitus.
- Imaging (MRI or CT Scan): Imaging is not standard for all tinnitus patients. It is typically ordered only when a specific structural cause is suspected. For example, an MRI is the gold standard for diagnosing an acoustic neuroma, especially if you have unilateral tinnitus. An MRA or CTA might be used to investigate vascular issues if you have pulsatile tinnitus.
What Tinnitus Treatments Actually Work?
Important Disclaimer: While there is currently no universal “cure” that can eliminate all forms of chronic tinnitus for every person, this does not mean that relief is impossible.
There are many highly effective, evidence-based management strategies that can significantly reduce the perception and impact of tinnitus, improving your quality of life.
Treatment is aimed at either addressing the underlying cause (if one is found) or, more commonly, helping you manage the symptom and your brain’s reaction to it.
Sound Therapies (Masking and Distraction)
The principle behind sound therapy is simple: a quiet environment makes tinnitus more noticeable.
By introducing other, more pleasant or neutral sounds, you can mask, distract from, or reduce the contrast of the tinnitus sound, making it less intrusive.
- Hearing Aids: For the majority of people with tinnitus who also have hearing loss, hearing aids are the most effective tool. They achieve two goals: they improve hearing and, by amplifying ambient sounds, they mask the tinnitus.
- Wearable Sound Generators: These are small devices that look like hearing aids but are designed to produce a continuous, low-level sound (like white noise or nature sounds) to mix with and reduce the prominence of the tinnitus.
- Tabletop Sound Machines & Smartphone Apps: Used often for sleep, these devices play a variety of soothing sounds (waves, rain, fans) to create a relaxing auditory environment that makes it easier to ignore tinnitus and fall asleep.
Behavioral Therapies (Retraining Your Brain’s Response)
Chronic tinnitus is not just an ear problem, it’s a brain problem.
The emotional reaction to the sound—the frustration, anxiety, and stress—is often more debilitating than the sound itself.
Behavioral therapies are designed to break this negative cycle.
- Cognitive Behavioral Therapy (CBT): CBT is one of the most well-researched and effective treatments for managing tinnitus distress. A therapist helps you identify negative thought patterns and emotional reactions to the tinnitus sound and teaches you techniques to reframe them. The goal isn’t to eliminate the sound, but to change your relationship with it so it no longer controls your life. A 2021 review by the American Academy of Family Physicians confirms CBT has a moderate- to high-quality evidence base for mitigating the effects of tinnitus.
- Tinnitus Retraining Therapy (TRT): TRT is a highly structured approach that combines low-level sound therapy with intensive counseling. The goal is habituation—to retrain the brain, both consciously and subconsciously, to reclassify the tinnitus sound as unimportant and filter it out, much like it filters out the sound of a refrigerator humming.
Lifestyle and Home Strategies
Simple changes to your daily routine can have a significant impact on tinnitus severity:
- Stress Management: Stress is a major tinnitus aggravator. Practices like mindfulness, meditation, yoga, and deep breathing can help calm the nervous system and reduce tinnitus perception.
- Reduce Stimulants: For some people, caffeine, alcohol, and nicotine can cause temporary spikes in tinnitus. Experimenting with reducing your intake can help determine if they are a trigger for you.
- Improve Sleep Hygiene: Tinnitus often seems louder at night. Establishing a consistent sleep schedule, ensuring your bedroom is dark and cool, and using a sound machine can promote better sleep.
- Protect Your Hearing: Even if you already have tinnitus, further noise damage can make it worse. Always use hearing protection in loud environments.
The Horizon: Can You Prevent Tinnitus?
While some causes of tinnitus, like age-related hearing loss or a rare tumor, cannot be prevented, the most common cause in younger and middle-aged adults—noise-induced hearing loss—is almost entirely preventable.
Empowering yourself with preventive strategies is the best defense against developing chronic tinnitus.
- Hearing Protection is Key: This cannot be overstated. If you work in a noisy industry, play a musical instrument, or use loud equipment like lawnmowers or power tools, make high-fidelity earplugs or industrial-grade earmuffs your constant companions.
- Turn Down the Volume: Be mindful of your headphone volume. A good rule of thumb is the 60/60 rule: listen at no more than 60% of the device’s maximum volume for no longer than 60 minutes at a time before taking a break. Invest in noise-cancelling headphones, which allow you to listen at lower volumes in noisy environments.
- Manage Cardiovascular Health: A healthy heart and healthy blood vessels mean a healthy blood supply to your ears. Regular exercise, a balanced diet, and managing your blood pressure and cholesterol can help prevent the vascular issues that lead to pulsatile tinnitus.
- Be Aware of Medication Risks: When starting a new medication, especially one from the ototoxic list, be vigilant for any changes in your hearing or the onset of tinnitus. Report any symptoms to your doctor immediately.
What’s New in Tinnitus Research?
The field of tinnitus research is more active than ever, moving away from the outdated notion that “nothing can be done” and toward innovative diagnostic and therapeutic approaches.
Here are some of the most exciting frontiers.
“Hidden Hearing Loss”: The Invisible Damage
One of the most significant recent breakthroughs comes from researchers at Harvard Medical School.
They are finding compelling evidence for a condition they call “hidden hearing loss”.
This refers to damage to the auditory nerve fibers that is not detected by a standard hearing test (audiogram).
A study published in Scientific Reports in late 2023 found that people with chronic tinnitus and “normal” hearing tests showed signs of auditory nerve degeneration.
This supports the theory that tinnitus can arise from this invisible damage, finally providing a potential explanation for the countless patients who were told their hearing was fine despite their persistent symptoms.
This research opens the door to developing new diagnostic tools and therapies aimed at regenerating these nerve fibers.
Bimodal Neuromodulation: Retraining the Brain with Dual Signals
A highly promising new category of treatment is bimodal neuromodulation.
This approach is based on the principle of neuroplasticity—the brain’s ability to reorganize itself.
These devices deliver two types of stimuli simultaneously to encourage the brain to “unlearn” the tinnitus signal.
The most prominent example is the Lenire device, which received FDA De Novo approval in 2023.
It combines sound stimulation through headphones with gentle electrical pulses delivered to the tongue via a small mouthpiece.
Large-scale clinical trials have shown that this dual stimulation can lead to significant and long-lasting reductions in tinnitus severity for many users.
Genetic Links and Personalized Medicine
Researchers are also exploring the genetic underpinnings of tinnitus.
Recent studies, including work from the Karolinska Institutet, suggest that certain forms of tinnitus, particularly severe cases that run in families, may have a hereditary component.
By identifying the specific genes involved, scientists hope to develop targeted drug therapies and personalized treatment plans, moving away from a one-size-fits-all approach and toward medicine tailored to an individual’s unique tinnitus profile.
Your Tinnitus Questions, Answered
1. Can stress cause tinnitus?
Stress does not directly cause tinnitus, but it is a major aggravator. High stress levels can trigger the body’s “fight or flight” response, which can make the brain’s perception of tinnitus more intense and your emotional reaction to it more severe, creating a vicious cycle.
2. Will my tinnitus ever go away?
Acute tinnitus, such as after a loud concert, often goes away on its own. Chronic tinnitus may not disappear completely, but its impact can be significantly reduced through effective management strategies like sound therapy and CBT to the point where it is no longer bothersome.
3. Can tinnitus cause hearing loss?
No, tinnitus is a symptom, not a cause. The relationship is the other way around: hearing loss is the most common cause of tinnitus. The tinnitus is the brain’s reaction to the hearing loss, not the cause of it.
4. Is there a vitamin that helps tinnitus?
There is no scientific evidence that any vitamin or supplement can cure tinnitus. While some companies market products with Ginkgo Biloba or B vitamins, studies have not proven their effectiveness. A balanced diet is always beneficial for overall health, including ear health.
5. Why is my tinnitus worse at night?
Your tinnitus isn’t necessarily getting louder at night, it’s just more noticeable. During the day, the ambient sounds of your environment partially mask the tinnitus. In the quiet of your bedroom, there is less external sound to compete with, making the tinnitus seem more prominent.
6. Can caffeine make tinnitus worse?
For some individuals, caffeine can act as a stimulant that temporarily increases the loudness of their tinnitus. However, this effect varies greatly from person to person. If you are a regular coffee drinker, suddenly stopping can also sometimes lead to withdrawal symptoms that worsen tinnitus.
7. Is it safe to use headphones if I have tinnitus?
Yes, it is safe as long as you are responsible with the volume. Listening at low to moderate levels can actually be helpful as a form of sound therapy. The danger comes from listening at high volumes, which can cause further hearing damage and worsen tinnitus.
8. What is the best sound to mask tinnitus for sleep?
The “best” sound is subjective. Many people find broadband sounds like white noise, pink noise, or brown noise to be effective. Others prefer nature sounds like gentle rain or ocean waves. The goal is to find a sound that is calming and effectively blends with your tinnitus.
9. Can dehydration cause ringing in the ears?
Yes, severe dehydration can potentially cause or worsen tinnitus. The fluid balance in the inner ear is delicate, and dehydration can disrupt it. It can also affect blood pressure and flow, which could contribute to tinnitus symptoms. Staying well-hydrated is important for overall health.
10. When should I be worried about my tinnitus?
You should see a doctor promptly if your tinnitus is: only in one ear (unilateral), pulsatile (in time with your heartbeat), accompanied by sudden hearing loss or vertigo, or is causing you significant anxiety or depression. These can be signs of a more serious underlying condition.
Conclusion and Next Steps
Tinnitus is a complex and deeply personal condition, but it is not an unsolvable mystery.
As we have explored, it has many potential causes, from the natural process of aging and the hazards of a noisy world to the side effects of medication and the symptoms of underlying health conditions.
The central message is one of hope and empowerment: understanding the specific trigger for your tinnitus is the definitive first step toward effective management and reclaiming your quality of life.
Relief is not found in a single magic bullet, but through a systematic process of diagnosis and a personalized management plan.
Whether through the use of hearing aids that restore the world of sound, behavioral therapies that retrain your brain’s response, or new technologies that leverage neuroplasticity, there are more effective pathways to relief available today than ever before.
If you are struggling with the persistent sound of tinnitus, the most important step you can take is to schedule an evaluation with an audiologist or an Ear, Nose, and Throat (ENT) specialist. A professional diagnosis is the key to unlocking the right management plan for you and ruling out any serious underlying medical issues.
Do you have a personal experience with tinnitus? Have you found a strategy that works for you?
Share your story or questions in the comments below to help others in the community who are on the same journey.
References
- National Institute on Deafness and Other Communication Disorders (NIDCD). (2023). Tinnitus.
- Mayo Clinic. (2022). Tinnitus – Symptoms and causes.
- American Tinnitus Association (ATA). Understanding the Facts.
- Apple Inc. (2024). Apple Hearing Study shares preliminary insights on tinnitus.
- Harvard Health Publishing. (2024). New thinking about tinnitus.
- Dalrymple, S. N., et al. (2021). Tinnitus: Diagnosis and Management. American Family Physician.
- Neuromod Devices Ltd. (2023). Neuromod Receives FDA De Novo Grant For Lenire Tinnitus Treatment Device.
- Alharthy, A. K. H., et al. (2024). Psychological Impact and Quality of Life in Adults With Tinnitus: A Cross-Sectional Study. Cureus.
- Karolinska Institutet. (2025). New knowledge on tinnitus gives hope.

