Plan B One-Step is an emergency contraceptive pill designed to prevent pregnancy after unprotected sex or contraceptive failure.
Its primary, scientifically-proven function is to delay or prevent ovulation, meaning it stops an egg from being released so fertilization cannot occur.
With nearly 1 in 4 sexually experienced women in the U.S. having used emergency contraception, its role in reproductive health is undeniable, according to data from the Guttmacher Institute.
Yet, despite its widespread use, significant misinformation persists about how it works, its effectiveness and its safety.
This article provides a comprehensive, evidence-based guide to help you understand the science behind Plan B, its true effectiveness and limitations (including crucial factors like timing and weight), potential side effects, and a practical guide to accessing and using it correctly.
Read on for a definitive guide to making an informed decision when you need it most.
In This Article
Key Points at a Glance
- What it is: Plan B is an emergency contraceptive, not a regular birth control method or an abortion pill.
- How it works: Its main function is to delay or prevent ovulation (the release of an egg).
- When to take it: As soon as possible within 72 hours (3 days) of unprotected sex for best results.
- Effectiveness: Highly effective, but this decreases over time and can be influenced by factors like body weight.
- Availability: Available over-the-counter in the U.S. without a prescription or age restriction.
Part 1: What is Plan B and When Should You Use It?
In moments of uncertainty following unprotected sex, understanding your options is the first step toward regaining control.
Plan B One-Step is the most well-known brand of emergency contraception (EC) in the United States, but what exactly is it, and when is its use appropriate?
This section provides the foundational, “need-to-know” information in a clear, direct and actionable format.
Defining Plan B One-Step: An Emergency Solution
At its core, Plan B One-Step is a brand name for a single pill containing 1.5 milligrams of a synthetic hormone called levonorgestrel.
Levonorgestrel is a type of progestin, a man-made version of the natural hormone progesterone, which plays a vital role in the menstrual cycle and pregnancy.
This same hormone is found in many lower-dose daily birth control pills.
It is crucial to understand the classification of Plan B. It is strictly an emergency contraceptive.
This means it is intended for occasional, backup use after a primary contraceptive method has failed or was not used.
It is not designed, nor is it as effective as, regular, ongoing contraceptive methods like birth control pills, IUDs or condoms.
A common and critical point of confusion is the difference between emergency contraception and an abortion pill (like mifepristone). Plan B works by preventing a pregnancy from starting. It does this primarily by stopping the ovary from releasing an egg. If you are already pregnant—meaning a fertilized egg has implanted in the uterus—Plan B will not work and will not harm the existing pregnancy. It is not an abortifacient.
Key Scenarios for Use
Emergency contraception is a second chance to prevent pregnancy.
The circumstances that might lead someone to consider Plan B are varied, but they all share a common thread: the risk of unintended pregnancy after recent sexual intercourse.
Here are the primary scenarios where using Plan B is indicated:
- Contraceptive Failure: This is one of the most common reasons for using EC. For example, a condom broke or slipped off during sex, or a diaphragm or cervical cap was dislodged.
- Missed Regular Birth Control Pills: Forgetting to take two or more combination birth control pills, or being late to start a new pack, can compromise their effectiveness and create a window of risk.
- Issues with Other Methods: A birth control patch falling off, forgetting to insert a new vaginal ring on time, or being late for a contraceptive injection (like Depo-Provera) are all valid reasons to consider EC.
- No Contraception Was Used: In situations where no form of birth control was used during vaginal intercourse.
- Forced or Non-Consensual Sex: In the traumatic event of sexual assault, emergency contraception is a critical medical option to prevent pregnancy.
In any of these situations, Plan B provides a safe and effective way to reduce the likelihood of pregnancy.
The Critical Time Window for Taking Plan B
The effectiveness of Plan B is directly tied to how quickly it is taken after unprotected intercourse.
The mantra for all levonorgestrel-based emergency contraception is: as soon as possible.
The U.S. Food and Drug Administration (FDA) has approved Plan B One-Step for use within 72 hours (3 days) of unprotected sex.
The clinical trials that established its safety and efficacy were based on this timeframe.
The sooner it’s taken within this window, the higher the chance of it working.
Some studies have suggested that levonorgestrel may still have some effect up to 120 hours (5 days) after intercourse, but its effectiveness drops significantly after the 72-hour mark.
For this reason, if more than three days have passed, other emergency contraception options, such as Ella or a copper IUD, may be more effective choices.
This will be discussed in detail in Part 6.
Think of the time window as a race. Sperm can live in the female reproductive tract for up to five days, waiting for an egg. Plan B’s job is to delay the release of that egg until the sperm are no longer viable. The sooner you take the pill, the more time you give it to successfully “pause” ovulation before it happens.
Part 2: How Does Plan B Work? A Deep Dive into the Science
To truly understand Plan B, we must look beyond the packaging and into the complex hormonal symphony of the human body.
The phrase “it prevents pregnancy” is accurate but simplistic. The real question is *how*.
This section delves into the biological mechanisms, clarifies the science, and directly addresses the persistent controversies surrounding its mode of action, establishing a level of expertise that goes far beyond a surface-level explanation.
The Primary Mechanism: Delaying Ovulation
The overwhelming scientific consensus, supported by decades of research and affirmed by major health bodies like the American College of Obstetricians and Gynecologists (ACOG) and the FDA, is that Plan B’s primary and most significant mechanism of action is the inhibition or delay of ovulation.
Understanding the Normal Ovulation Process
To grasp how Plan B intervenes, one must first understand the normal process it disrupts.
The menstrual cycle is governed by a delicate feedback loop of hormones.
In the days leading up to ovulation, a hormone called Follicle-Stimulating Hormone (FSH) encourages a follicle (a small sac containing an egg) in the ovary to mature.
As the follicle grows, it produces estrogen.
When estrogen levels reach a certain peak, it triggers a rapid, massive release of another hormone from the brain’s pituitary gland: the Luteinizing Hormone (LH).
This is known as the LH surge. The LH surge is the direct, non-negotiable trigger for ovulation.
Approximately 24 to 36 hours after the LH surge begins, the mature follicle ruptures, releasing the egg into the fallopian tube. This is ovulation.
How Levonorgestrel Intervenes
Plan B introduces a high dose of the synthetic progestin, levonorgestrel.
When taken *before* the LH surge has begun, this powerful dose of progestin acts on the brain (specifically the hypothalamus and pituitary gland) to block the LH surge from happening.
Without the LH surge, the follicle does not receive the signal to rupture. Ovulation is postponed for several days.
Analogy: Imagine the LH surge is the “launch” command for the egg. Levonorgestrel effectively cuts the communication line from mission control (the brain) to the launchpad (the ovary). The launch is scrubbed. By the time the body’s natural hormone levels reset and ovulation eventually occurs a few days later, any sperm from the unprotected intercourse are no longer viable (sperm typically survive for a maximum of 5 days). Therefore, there is no egg for the sperm to fertilize and pregnancy is averted.
This is why timing is so critical.
If Plan B is taken after the LH surge has already started, or after ovulation has already occurred, it cannot stop the process.
It has no effect on an egg that has already been released, which is why it is not 100% effective.
Secondary Mechanisms: A Supporting Role
While delaying ovulation is the star of the show, research has explored other potential ways levonorgestrel might contribute to preventing pregnancy, though these are considered minor or less consistent effects.
Thickening Cervical Mucus
Progestins are known to alter the consistency of the mucus produced by the cervix.
The high dose of levonorgestrel in Plan B can make this mucus thicker and more viscous.
This change can create a physical barrier that impairs sperm motility, making it more difficult for sperm to swim through the cervix and into the uterus and fallopian tubes to reach an egg.
While this effect is well-documented with continuous progestin use (like in mini-pills), its significance in a single emergency dose is less certain but considered a plausible secondary contribution.
Addressing the Controversy: Does Plan B Prevent Implantation?
This is perhaps the most contentious and misunderstood aspect of Plan B.
The question is whether Plan B can work *after* fertilization by preventing the newly formed embryo from implanting in the uterine wall.
This potential mechanism is often referred to as *interception* and is at the heart of the ethical and moral debates surrounding the pill.
The Evolution of Scientific Understanding
For many years, the product labeling for Plan B included a line stating that it “may inhibit implantation”.
This language was included in the original FDA approval because, at the time, the full range of mechanisms was not perfectly understood, and a post-fertilization effect could not be definitively ruled out.
This created a window of ambiguity that fueled controversy.
However, over the past two decades, more sophisticated research has provided a much clearer picture.
A large body of evidence has failed to demonstrate any significant effect of levonorgestrel on the endometrium (the lining of the uterus) that would make it hostile to implantation.
A landmark review of studies published in the journal Contraception concluded that “evidence is accumulating that LNG-ECPs are not abortifacient”.
The most compelling evidence comes from studies, like one detailed in an NCBI-archived article, that precisely timed the administration of levonorgestrel in relation to ovulation.
These studies consistently show that when the pill is given on or after the day of ovulation, it does not reduce the pregnancy rate compared to what would be expected without any treatment.
If it worked by preventing implantation, it should still be effective even if taken after ovulation.
The fact that it isn’t is strong evidence that its effects are pre-fertilization.
The Official Stance: FDA Label Update
In recognition of this overwhelming scientific consensus, the FDA announced in December 2022 that it was updating the product information for Plan B One-Step.
The new labeling clarifies that the primary mechanism is preventing or delaying ovulation and removes the speculative language about inhibiting implantation.
“Plan B One-Step works before release of an egg from the ovary. As a result, Plan B One-Step prevents pregnancy primarily by stopping the release of an egg from the ovary (ovulation), it may also prevent the fertilization of an egg (the uniting of sperm with the egg) if ovulation has already occurred”. – FDA Statement
This official change reflects the modern scientific understanding: Plan B is not an abortion pill and there is no reliable evidence that it works by preventing implantation of a fertilized egg.
It works by preventing fertilization from happening in the first place.
Scientific Distinction: Contraception vs. Interception
To demonstrate a deep understanding of this topic, it’s helpful to clarify the terminology:
- Contraception: Any method or device that serves to prevent fertilization. This includes barrier methods (condoms), hormonal methods that prevent ovulation (birth control pills, Plan B), and methods that are toxic to sperm (spermicide, copper IUD).
- Interception: A theoretical mechanism that would act after fertilization but before or during implantation. This is what opponents sometimes inaccurately attribute to Plan B.
- Abortifacient: A substance that induces the termination of an established pregnancy (i.e., after implantation has occurred).
Based on current evidence, Plan B is firmly in the category of a contraceptive.
Part 3: How Effective is Plan B? The Real Numbers and Influencing Factors
After “how does it work?”, the most urgent question is “will it work?”.
The effectiveness of Plan B is not a single, simple number. It’s a dynamic probability influenced by several critical variables.
This section breaks down the data, presents it in an easy-to-understand format, and explores the two most important factors—timing and body weight—that can significantly alter its success rate.
Understanding the Effectiveness Rate
Manufacturers and health organizations often state that Plan B and its generics can reduce the risk of pregnancy by 75-89% when taken within 72 hours.
While this is a helpful benchmark, it’s an average.
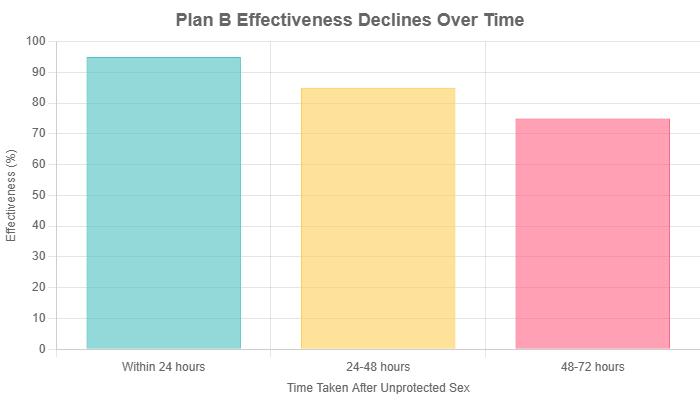
The true effectiveness is highest in the first 24 hours and declines with each passing day.
A more granular look at the data provides a clearer picture of this time-dependent efficacy.
While exact percentages can vary slightly between studies, the general trend is consistent and dramatic.
Effectiveness by Time Taken
The following table and chart illustrate the estimated effectiveness of levonorgestrel emergency contraception based on when it is taken after unprotected sex.
These figures represent the reduction in the number of expected pregnancies.
| Time Taken After Unprotected Sex | Estimated Effectiveness (Pregnancy Risk Reduction) |
|---|---|
| Within 24 hours | Up to 95% |
| Between 24-48 hours | Approximately 85% |
| Between 48-72 hours | Approximately 75% |
| After 72 hours (3 days) | Significantly lower and not recommended |
The Crucial Caveat: Your Menstrual Cycle
It is absolutely critical to understand that these effectiveness rates are not guaranteed.
The single most important factor determining if Plan B will work is where you are in your menstrual cycle.
As explained in Part 2, Plan B works by stopping ovulation. Therefore:
- If you have unprotected sex and take Plan B several days before you are set to ovulate, it is highly likely to be effective.
- If you have unprotected sex on the day of ovulation or the day after, and you take Plan B, it will not be effective because the egg has already been released. The pill cannot “un-release” an egg.
Since many people do not know the exact day they ovulate, taking the pill as soon as possible provides the best statistical chance of it intervening before the LH surge and subsequent ovulation occur.
Factor 1: Body Weight and BMI
A growing body of research has identified a significant factor that can influence Plan B’s effectiveness: a person’s body weight or Body Mass Index (BMI).
This is a critical point of information that is often overlooked in basic explanations of the pill.
The Scientific Evidence
Multiple studies have suggested that levonorgestrel-based emergency contraception, including Plan B, may be less effective for individuals with a higher BMI. The general findings indicate:
- For individuals with a BMI over 25 (classified as overweight), the effectiveness of Plan B may be reduced.
- For individuals with a BMI over 30 (classified as obese), some studies suggest Plan B may not be effective at all, with pregnancy rates similar to taking no emergency contraception.
The reason for this is believed to be pharmacokinetic.
The 1.5 mg dose of levonorgestrel is a fixed amount. In a person with a larger body mass and higher blood volume, the hormone becomes more diluted.
This can result in a lower peak concentration of the drug in the bloodstream, which may be insufficient to reliably block the LH surge and prevent ovulation.
A 2011 study published in Contraception was one of the first to highlight this, finding that the risk of pregnancy was more than three times higher for obese women using levonorgestrel EC compared to women with a normal BMI.
What Are the Alternatives?
This information is not meant to cause panic, but to empower individuals to choose the most effective option for their body.
If you have a BMI over 25, and especially if it’s over 30, you should be aware that Plan B may not be your most reliable choice. The recommended alternatives are:
- Ella (Ulipristal Acetate): This is another type of emergency contraception pill. Studies have shown that Ella maintains its effectiveness in individuals with a BMI up to 35. It is available by prescription only in the United States.
- Copper IUD (Intrauterine Device): The copper IUD is the most effective form of emergency contraception available, reducing the risk of pregnancy by over 99.9%. Its effectiveness is not affected by body weight. It must be inserted by a healthcare provider within 5 days of unprotected sex. As a bonus, it can then be left in place to provide highly effective, long-term contraception for up to 10-12 years.
If you are concerned about your weight impacting Plan B’s effectiveness, the best course of action is to contact a healthcare provider or a clinic like Planned Parenthood as soon as possible to discuss obtaining a prescription for Ella or an appointment for a copper IUD.
Factor 2: Drug Interactions
Just like many other medications, the efficacy of Plan B can be compromised by other drugs or supplements that affect how it is metabolized by the body.
Certain substances, known as enzyme inducers, can speed up the breakdown of levonorgestrel in the liver, clearing it from the bloodstream too quickly for it to work properly.
It is vital to be aware of these potential interactions.
If you are taking any of the following medications, Plan B may be less effective:
- The antibiotic Rifampin (and related rifamycin drugs). It’s important to note that other common antibiotics, like those used for UTIs or strep throat, do not interfere with Plan B.
- The antifungal Griseofulvin.
- Certain anti-seizure medications (antiepileptics), including barbiturates, carbamazepine (Tegretol), phenytoin (Dilantin), primidone and oxcarbazepine.
- Certain medications used to treat HIV, such as efavirenz.
- The herbal supplement St. John’s Wort, which is often used for depression.
Actionable Advice for Drug Interactions
If you are taking one of these interacting medications, you have a few options, and you should act quickly:
- Consult a Pharmacist or Doctor Immediately: A pharmacist is an excellent and accessible resource. They can review your full medication list and provide immediate advice.
- Consider a Higher Dose: Some guidelines suggest that taking a double dose of levonorgestrel (3.0 mg) might overcome the interaction, but this should only be done under the guidance of a healthcare professional.
- Opt for a Different EC Method: The most reliable solution is to use a method unaffected by these drugs. The copper IUD is the best choice, as its mechanism is localized in the uterus and is not impacted by liver metabolism. Ella may also be an option, but it can also be affected by some of these drugs, so a professional consultation is essential.
Part 4: Plan B Side Effects: What to Expect and When to Worry
Beyond effectiveness, safety is a primary concern.
Plan B is considered extremely safe by medical experts, and serious complications are very rare.
However, the high dose of hormone can cause some temporary and generally mild side effects.
Understanding what is normal, what to do about it, and when to seek medical attention is key to navigating the experience with confidence.
Common Side Effects: Insights from Clinical Trials
The side effects of Plan B are primarily caused by the sudden influx of a large dose of progestin.
These effects are usually short-lived, lasting only a day or two.
Data from the original FDA clinical trials provide a clear picture of how common these side effects are.
The most frequently reported include:
- Menstrual Changes (Heavier or Irregular Bleeding): This is the most common side effect, reported by about 31% of users in clinical trials.
- Nausea: Experienced by approximately 14% of users. This is less common than with older, estrogen-containing EC pills.
- Lower Abdominal Pain or Cramps: Reported by about 13% of users.
- Fatigue: Also reported by about 13% of users.
- Headache: Experienced by roughly 10% of users.
- Dizziness: A less common, but possible, side effect.
- Breast Tenderness: The hormonal shift can cause temporary breast sensitivity, similar to what some experience before their period.
It’s important to remember that many people experience no side effects at all.
If you do experience them, they are typically mild and resolve on their own within 48 hours.
Your Next Period: What’s Normal?
The most common source of anxiety after taking Plan B is its effect on your menstrual cycle.
Because the pill works by disrupting your natural hormonal rhythm, changes to your next period are very common and should be expected.
- Timing: It’s normal for your next period to arrive up to a week earlier or a week later than you would typically expect. Most people get their period within the expected timeframe, but a delay is not automatically a sign of pregnancy.
- Flow: The flow of your period might also be different. It could be heavier or lighter than usual.
- Spotting: Some people experience light, irregular bleeding or “spotting” in the days or weeks after taking Plan B, before their actual period begins. This is also a normal consequence of the hormonal disruption.
Clear Guidance on Pregnancy Testing
While a delayed period is normal, a significant delay can be a sign the pill did not work.
The standard medical advice is: If your period is more than one week late from its expected date, you should take a home pregnancy test to be sure.
What to Do If You Vomit
This is a simple but crucial instruction.
The pill needs time to be absorbed into your bloodstream through your digestive system.
If you vomit shortly after taking it, the medication may be expelled before it has a chance to work.
The 2-Hour Rule: If you vomit within 2 hours of taking the Plan B pill, it is likely that it was not fully absorbed. You should contact a doctor or pharmacist immediately. They will most likely advise you to take another dose. If you vomit more than 2 hours after taking the pill, it has likely been absorbed, and you do not need to take another one.
If you are prone to nausea, you might consider taking the pill with a light snack or an over-the-counter anti-nausea medication like meclizine, but consult a pharmacist first.
When to Contact a Doctor: Recognizing Red Flags
While serious complications are rare, it’s important to distinguish normal, transient side effects from symptoms that could indicate a more serious issue.
You should contact a healthcare provider right away if you experience any of the following after taking Plan B:
- Severe Lower Abdominal Pain: While mild cramping can be a normal side effect, sharp, persistent, or one-sided severe pain could, in very rare cases, be a sign of an ectopic pregnancy. An ectopic pregnancy is a non-viable pregnancy that implants outside the uterus (usually in a fallopian tube) and is a medical emergency. While Plan B does not cause ectopic pregnancies, it does not prevent them. If fertilization occurred and you were already at risk for an ectopic pregnancy, that risk remains.
- Heavy, Prolonged Bleeding: If you are soaking through more than two pads or tampons per hour for several hours in a row.
- No Period Within Three Weeks: If your period hasn’t arrived within three weeks of taking the pill, it’s essential to take a pregnancy test and follow up with a doctor regardless of the result.
- Signs of an Allergic Reaction: Though extremely rare, symptoms like hives, difficulty breathing, or swelling of the face, lips, or tongue require immediate emergency medical attention.
Your Practical Guide to Getting and Using Plan B
In a stressful situation, the last thing you need are barriers to access.
Fortunately, in the United States, obtaining Plan B has become relatively straightforward.
This section provides a practical, step-by-step guide on where to find it, what to expect in terms of cost, and how to navigate the process with confidence.
Where to Buy Plan B (No Prescription Needed)
A major step forward in reproductive health access was the FDA’s decision to make levonorgestrel-based emergency contraception available over-the-counter (OTC).
This means you do not need to see a doctor or get a prescription to purchase it.
In the U.S., there are no age or gender restrictions for purchasing Plan B One-Step or its generic equivalents.
You can find it in a variety of locations:
- Drugstores and Pharmacies: National chains like CVS, Walgreens, and Rite Aid, as well as independent local pharmacies, all carry emergency contraception.
- Supermarkets and Big-Box Stores: Large retailers with pharmacy sections, such as Walmart, Target, Costco, and major grocery store chains, typically stock it.
- Online Retailers: You can purchase Plan B and generics online from services like Amazon or specific EC providers. However, this is only a viable option for future preparedness, not for immediate need, due to shipping times.
- Family Planning Clinics: Organizations like Planned Parenthood and local health department clinics are excellent resources. They not only provide the medication but can also offer counseling and answer any questions you may have.
Important Note on Location in the Store
Even though it’s OTC, you might not find Plan B on a regular shelf next to the pain relievers.
Due to its cost and to prevent theft, many stores keep it behind the pharmacy counter or in a locked plastic case on the shelf.
You may need to ask a pharmacist or store employee for assistance.
Remember, you do not need to show ID or have a prescription to ask for it.
Plan B Cost: Brand vs. Generic
The cost of emergency contraception can be a significant barrier for some.
The price can vary widely depending on the brand and the location of purchase.
- Brand-Name Plan B One-Step: The original brand-name product is typically the most expensive, usually costing between $40 and $50.
- Generic Versions: There are numerous FDA-approved generic versions that are chemically identical to Plan B One-Step. Common brand names for these generics include Take Action, My Way, Aftera, My Choice, and EContra EZ. These are significantly more affordable, generally ranging from $11 to $45.
Key takeaway: All 1.5 mg levonorgestrel pills are bioequivalent and work the exact same way. There is no medical reason to choose the more expensive brand-name Plan B over a more affordable generic version. The active ingredient and dose are identical.
Can You Get Plan B for Free?
Yes, for many people, it is possible to get emergency contraception at no cost or a reduced cost.
Here are the primary avenues to explore:
- Health Insurance: Under the Affordable Care Act (ACA), most insurance plans are required to cover all FDA-approved contraceptive methods, including emergency contraception, with no copay. Even though Plan B is available over-the-counter, you may need to get a prescription from a doctor for your insurance to cover the cost. You can call your doctor’s office and ask for a prescription to be sent to your pharmacy.
- Medicaid: If you are covered by Medicaid, it will also typically cover the cost of emergency contraception with a prescription.
- Clinics and Health Departments: Local health departments and family planning clinics (like Planned Parenthood) often provide emergency contraception on a sliding scale based on your income, and in some cases, for free. This is an excellent option if you are uninsured or prefer not to use insurance.
Expert Tip: Be Prepared
One of the most empowering actions you can take for your reproductive health is to be proactive.
The effectiveness of Plan B hinges on taking it as soon as possible.
The stress of a contraceptive failure is compounded by the frantic rush to find an open pharmacy and purchase the pill.
A simple solution is to buy an emergency contraceptive pill before you need it and keep it in your medicine cabinet.
Levonorgestrel pills have a shelf life of several years.
Having one on hand means you can take it immediately if an accident happens, maximizing its effectiveness and minimizing your stress.
This simple act of preparation can make a world of difference in a critical moment.
Part 6: Plan B vs. Other Emergency Contraception
While Plan B is the most well-known name in emergency contraception, it is not the only option.
Understanding the full landscape of available methods is crucial for making the best choice for your specific situation, especially when factors like time passed or body weight are a concern.
This section provides a head-to-head comparison of the three main types of EC available in the U.S.
A Detailed Comparison of Your Options
The three primary methods of emergency contraception are the levonorgestrel pill (Plan B and generics), the ulipristal acetate pill (Ella), and the copper IUD.
Each has a different mechanism, time window, and effectiveness profile.
| Feature | Plan B (Levonorgestrel) | Ella (Ulipristal Acetate) | Copper IUD (ParaGard) |
|---|---|---|---|
| Type | Progestin-only pill | Progesterone agonist/antagonist pill | Non-hormonal intrauterine device |
| How it Works | Primarily delays or inhibits ovulation by blocking the LH surge. | Delays ovulation, even when the LH surge has begun. It is a selective progesterone receptor modulator. | Copper ions are toxic to sperm and prevent fertilization. May also prevent implantation, though this is not its primary EC mechanism. |
| Time Window | Labeled for use up to 72 hours (3 days). Best results within 24 hours. Some effect up to 5 days. | Consistently effective for up to 120 hours (5 days). | Highly effective for up to 120 hours (5 days). |
| Effectiveness | Good (Reduces pregnancy risk by 75-95%, depending on timing). | Very High (Reduces pregnancy risk by ~98-99%). Considered more effective than Plan B, especially on days 4 and 5. | Highest (Reduces pregnancy risk by >99.9%). The most effective EC method. |
| Impact of BMI | Effectiveness may be reduced in individuals with a BMI > 25 and may be ineffective if BMI > 30. | Maintains effectiveness better than Plan B at higher BMIs, up to a BMI of 35. | Effectiveness is not affected by body weight or BMI. |
| Availability | Over-the-counter (OTC). No prescription needed. | Prescription only in the United States. | Must be inserted by a trained healthcare provider. |
| Long-Term Use | No. For emergency use only. | No. For emergency use only. | Yes. Can be left in place for up to 10-12 years as highly effective, long-term contraception. |
Key Takeaways: Choosing the Right EC for You
This comparison makes it clear that the “best” emergency contraceptive depends on your individual circumstances.
When Plan B is a Great Choice:
Plan B is an excellent and highly accessible option if it has been less than 3 days since unprotected sex, and you do not have a high BMI or are not taking any interacting medications.
Its OTC availability makes it the fastest and easiest option to obtain for most people.
When Ella Might Be a Better Choice:
You should strongly consider contacting a doctor for a prescription for Ella if:
- It has been more than 3 days (72 hours) but less than 5 days (120 hours) since unprotected sex. Ella maintains its high effectiveness throughout this entire window.
- You have a BMI between 25 and 35. Ella has been shown to be more effective than Plan B in this weight range.
Note: You should not take Plan B and Ella within the same cycle, as they can interfere with each other.
Also, you should wait 5 days after taking Ella before starting or resuming hormonal birth control.
When the Copper IUD is the Superior Choice:
The copper IUD is the gold standard of emergency contraception and should be considered if:
- You want the most effective method possible, regardless of other factors.
- It has been up to 5 days since unprotected sex.
- Your BMI is over 30, as its effectiveness is not impacted by weight.
- You are interested in a highly effective, non-hormonal, long-term birth control method. Getting it for an emergency can solve two problems at once.
The main barriers to the copper IUD are the need for a timely appointment with a healthcare provider for insertion and the upfront cost, though it is often covered by insurance.
Part 7: Frequently Asked Questions (FAQ)
Here are direct, concise answers to some of the most common questions people have about Plan B.
1. Does Plan B cause an abortion?
No. Scientific evidence shows Plan B works by preventing pregnancy from occurring, primarily by stopping ovulation so fertilization cannot happen. It does not interrupt or end an established pregnancy (one that has implanted in the uterus).
2. Will Plan B affect my future fertility?
No. There is no evidence that using emergency contraception, including Plan B, has any negative long-term impact on your ability to get pregnant in the future. Its effects are temporary and do not affect your underlying fertility.
3. Can I take Plan B if I’m already on birth control?
Yes. Plan B is often used as a backup in cases of birth control failure, such as missing several pills or a condom breaking. After taking Plan B, you should consult your pill’s instructions or a doctor about when to resume your regular pills.
4. How many times can I take Plan B?
While it is medically safe to take Plan B more than once, even within the same cycle, it is not recommended as a primary form of birth control. It is less effective than regular methods, and frequent use can lead to significant menstrual cycle disruption and more side effects.
5. Does Plan B protect against STIs?
No, absolutely not. Plan B only helps prevent pregnancy. It offers zero protection against sexually transmitted infections (STIs) like HIV, chlamydia or gonorrhea. Only barrier methods, such as condoms, can reduce the risk of STIs.
6. What happens if I take Plan B and I’m already pregnant?
If you take Plan B when you are already pregnant (even if you don’t know it yet), studies show that it will not harm the developing fetus or the pregnancy. The pill simply will not have any effect.
7. Can I take Plan B while breastfeeding?
Yes. According to the CDC and other health authorities, it is considered safe to take levonorgestrel-based emergency contraception while breastfeeding. Small amounts of the hormone may pass into breast milk, but it is not considered harmful to the baby.
8. How do I know if Plan B worked?
The only definitive way to know if Plan B worked is to wait for your next menstrual period. If your period arrives at or around its expected time, the pill was successful. If your period is more than one week late, you should take a pregnancy test.
Conclusion
Navigating the world of reproductive health can be complex, but understanding your options is a powerful tool.
Plan B One-Step and its generic equivalents represent a safe, accessible, and effective method of emergency contraception for millions.
Its power lies in its ability to act as a crucial backup, providing a second chance to prevent an unintended pregnancy.
Summary of Key Points
Throughout this guide, we have established that Plan B works primarily by delaying ovulation, a mechanism that prevents fertilization from ever occurring.
Its effectiveness is highest when taken as soon as possible after unprotected sex and can be limited by crucial factors like a person’s body weight and interactions with other medications.
While it can cause temporary side effects like nausea or changes to the menstrual cycle, it is overwhelmingly safe and does not impact future fertility.
Crucially, we have also clarified that Plan B is not an abortion pill and is distinct from other emergency options like Ella and the copper IUD, which may be more suitable choices in specific circumstances.
The ultimate goal is not to rely on Plan B as a primary method, but to know it exists as a reliable safety net, supported by science.
This article is intended to be a comprehensive source of information, but it cannot replace professional medical advice.
If you have any doubts, personal health concerns, or questions about which emergency contraception method is right for you, the best course of action is to speak with a healthcare provider or a pharmacist.
They can provide personalized advice based on your specific health history and situation, ensuring you make the safest and most effective choice.
Knowledge is a shared resource. Have a question we didn’t answer? Share your experience or ask in the comments below to help our community learn together. Your story could be the information someone else is searching for.
Reference
[1] How Effective Is Plan B? Here’s What Experts Say
[2] Emergency contraception – A narrative review of literature
https://www.sciencedirect.com/science/article/pii/S0301211524003038
[3] Levonorgestrel – StatPearls
https://www.ncbi.nlm.nih.gov/books/NBK539737
[4] Plan B One-Step (1.5 mg levonorgestrel) Information – FDA
[5] Mechanism of action of levonorgestrel emergency contraception
https://pmc.ncbi.nlm.nih.gov/articles/PMC4313438
[6] Plan B (Morning-After Pill): How it Works, Side Effects – Drugs.com
https://www.drugs.com/plan-b.html
[7] Levonorgestrel emergency contraception – Fertility and Sterility
https://www.fertstert.org/article/S0015-0282(06)04732-7/pdf
[8] [PDF] Plan B One-Step (levonorgestrel) Tablet – accessdata.fda.gov
https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/021998lbl.pdf
[9] Emergency Contraception
https://www.cdc.gov/contraception/hcp/usspr/emergency-contraception.html
[10] Maximizing the effectiveness of 1.5 mg levonorgestrel for …
https://www.sciencedirect.com/science/article/pii/S2590151624000042
[11] The FDA Declares Levonorgestrel a Nonabortifacient – JAMA Network
https://jamanetwork.com/journals/jama-health-forum/fullarticle/2807903

