Effectively treating a yeast infection depends on whether it’s uncomplicated or complicated, with options ranging from over-the-counter (OTC) creams to prescription oral medications.
This common condition, while rarely serious, can cause significant discomfort and disruption. Understanding your treatment choices is the first step toward finding fast and lasting relief.
It’s a remarkably common issue. According to the U.S. Office on Women’s Health, up to 75% of women will experience at least one yeast infection in their lifetime, and nearly half will have two or more.
This prevalence highlights the need for clear, reliable information to navigate the path to recovery.
This guide will provide a comprehensive overview of everything you need to know. We will explore how to confidently identify a yeast infection, conduct a deep dive into the differences between OTC and prescription treatments, and offer expert guidance for managing recurrent infections.
Furthermore, we’ll clarify how to distinguish a yeast infection from other common conditions like Bacterial Vaginosis (BV) and Urinary Tract Infections (UTIs).
Continue reading for a clear, evidence-based roadmap to help you make an informed decision about your health.
In This Article
What Exactly Is a Vaginal Yeast Infection?
A vaginal yeast infection, known medically as vaginal candidiasis, is a type of fungal infection that causes irritation, discharge, and intense itchiness of the vagina and the vulva (the tissues at the vaginal opening).
It’s a common condition that affects millions of women each year.
The infection is caused by an overgrowth of a type of yeast—a microscopic fungus—called Candida.
The most common culprit is a specific species named Candida albicans. It’s important to understand that Candida is a normal resident of the human body. It lives harmlessly in small numbers in the mouth, throat, gut, and vagina, coexisting with a host of other microorganisms.
The vaginal environment, or microbiome, is a delicate ecosystem. It’s naturally maintained in a state of balance by beneficial bacteria, most notably a group called Lactobacillus.
These “good” bacteria produce acid, which helps prevent the overgrowth of yeast and other potentially harmful organisms.
A yeast infection occurs when this delicate balance is disrupted, allowing Candida to multiply unchecked and invade deeper layers of vaginal tissue, leading to the classic symptoms of an infection.
A key point of clarification: A vaginal yeast infection is not considered a sexually transmitted infection (STI). Women who are not sexually active can get them. However, sexual activity can sometimes trigger an infection or spread it between partners, but it is not the primary mode of acquisition.
What Are the Telltale Symptoms of a Yeast Infection?
Recognizing the symptoms of a yeast infection is the first step toward getting the right treatment.
While symptoms can vary in intensity from mild to moderate, they typically share a distinct set of characteristics.
If you are experiencing a combination of the following, a yeast infection is a likely cause:
- Intense Itching and Irritation: This is often the most prominent and bothersome symptom, affecting the vagina and the surrounding vulvar area.
- Thick, White Vaginal Discharge: A hallmark sign is a discharge that is typically odorless and has a clumpy, white appearance, often compared to cottage cheese.
- Burning Sensation: You may experience a burning feeling, which can be particularly noticeable during urination or sexual intercourse. This is caused by urine or friction on the inflamed, sensitive tissues.
- Redness and Swelling: The vulva may appear red, swollen, and inflamed. On darker skin tones, the redness may be less apparent, but swelling and irritation will still be present.
- Vaginal Pain and Soreness: A general feeling of soreness or pain in the vaginal area is common.
- Small Cuts or Fissures: In more severe cases, the intense itching and inflammation can lead to tiny, painful cracks in the skin of the vulva.
It’s crucial to note that not everyone will experience all of these symptoms.
The presentation can differ from person to person and from one infection to another.
If this is your first time experiencing these symptoms, a professional diagnosis is essential to rule out other conditions.
What Causes a Yeast Infection to Develop?
A yeast infection is fundamentally an issue of imbalance. It develops when the natural environment of the vagina is altered, allowing the normally harmless Candida yeast to proliferate.
Several factors can trigger this disruption. Understanding these triggers is key to both treatment and prevention.
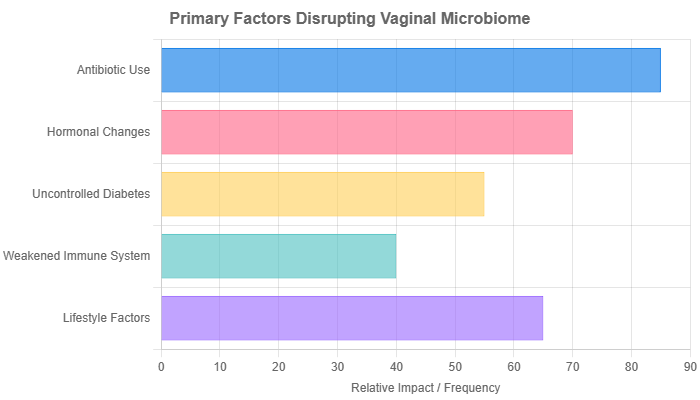
The most common risk factors that disrupt the vaginal microbiome include:
- Antibiotic Use: Broad-spectrum antibiotics are a primary culprit. While they are effective at killing harmful bacteria causing an illness, they don’t discriminate and also wipe out the beneficial Lactobacillus bacteria in the vagina. This removes the natural “gatekeepers,” allowing yeast to flourish.
- Hormonal Changes: Elevated levels of the hormone estrogen can promote the growth of Candida. This is why yeast infections are more common during certain life stages or with the use of certain medications, including:
- Pregnancy
- Birth control pills that contain higher doses of estrogen
- Hormone replacement therapy (HRT)
- Uncontrolled Diabetes: High blood sugar levels are not just in the blood; they are also present in the secretions of the vagina. Yeast feeds on sugar, so an environment rich in glucose provides an ideal breeding ground for Candida overgrowth.
- Weakened Immune System: A compromised immune system has a harder time keeping yeast in check. This can be due to conditions like HIV or the use of immunosuppressant medications, such as corticosteroids or chemotherapy.
- Lifestyle and Hygiene Habits: Certain daily habits can increase your risk by creating a warm, moist environment where yeast thrives. These include:
- Douching: This practice flushes out both good and bad bacteria, disrupting the natural pH and protective balance of the vagina.
- Scented Feminine Products: Perfumed sprays, pads, tampons, and bubble baths can irritate the delicate vaginal tissues and alter the pH.
- Staying in Wet Clothing: Lingering in a wet swimsuit or sweaty workout clothes for extended periods creates the perfect warm, damp conditions for yeast growth.
- Tight, Non-Breathable Clothing: Synthetic fabrics and tight-fitting pants can trap heat and moisture, contributing to an environment conducive to infection.
How Do I Know if I Can Treat a Yeast Infection at Home?
The pharmacy aisle offers a range of over-the-counter (OTC) treatments, but they aren’t suitable for everyone or every situation.
Making the right choice between self-treatment and seeing a doctor is critical for effective relief and long-term health.
This decision hinges on whether your infection is classified as uncomplicated or complicated.
When OTC Treatment is Likely Appropriate (Uncomplicated Infection)
You can likely manage the infection at home with an OTC product if you meet all of the following criteria:
- You’ve had a doctor diagnose you before. You are confident you can recognize the telltale symptoms of a yeast infection because a healthcare provider has diagnosed you with one in the past.
- Your symptoms are mild to moderate. You are experiencing the classic itching and cottage cheese-like discharge, but it’s not severe.
- You are not pregnant. Yeast infections during pregnancy require medical supervision.
- You are certain it’s not an STI. You have no reason to suspect you’ve been exposed to a sexually transmitted infection.
When You MUST See a Doctor (Complicated Infection or Uncertainty)
It is essential to schedule an appointment with a healthcare provider instead of self-treating if any of the following apply to you:
- This is your first-ever yeast infection. The symptoms of a yeast infection can mimic other, more serious conditions. A proper diagnosis is crucial to ensure you’re treating the right problem.
- You are pregnant or breastfeeding. Your doctor needs to recommend a treatment that is safe for you and your baby.
- You have recurrent infections. If you’ve had four or more yeast infections in a single year, you have what’s known as Recurrent Vulvovaginal Candidiasis (RVVC), which requires a specific medical management plan.
- Your symptoms are severe. This includes extensive redness, swelling, and itching that leads to cracks, tears, or sores in the vaginal tissue.
- You have an underlying health condition. If you have uncontrolled diabetes or a weakened immune system (e.g., from HIV or medication), you need medical guidance.
- Your symptoms don’t improve after using an OTC treatment. If you’ve completed a full course of OTC medication and are still experiencing symptoms, you may have a resistant strain of yeast or a different condition altogether.
Expert Tip: When in doubt, see a doctor. Misdiagnosing your condition can delay proper treatment and potentially worsen the underlying issue.
What Are My Over-the-Counter (OTC) Treatment Options?
If you’ve determined that an OTC treatment is appropriate for your situation, you’ll find several options available at your local pharmacy.
These treatments are all topical antifungals, meaning they are applied directly to the affected area. They belong to a class of drugs called “azoles.”
Common OTC Antifungals (Miconazole, Clotrimazole, Tioconazole)
The active ingredients in most OTC yeast infection treatments are highly effective against the common Candida albicans strain.
You’ll find them under various brand names, with Monistat being one of the most well-known, but store brands are equally effective if they contain the same active ingredient.
- Miconazole (e.g., Monistat)
- Clotrimazole (e.g., Gyne-Lotrimin)
- Tioconazole (e.g., Vagistat-1)
These medications come in several forms, often packaged as combination packs that include both an internal and external treatment:
- Vaginal Creams or Ointments: These are inserted into the vagina using a supplied applicator.
- Vaginal Suppositories: These are solid, oval-shaped inserts (ovules) that you place into the vagina, where they dissolve and release the medication.
- External Creams: Most kits include a small tube of cream to apply to the vulva to relieve external itching and burning.
Choosing a Treatment Length: 1, 3, or 7-Day Regimens
One of the main choices you’ll face at the pharmacy is the duration of the treatment: 1-day, 3-day, or 7-day regimens.
It’s a common misconception that one is “stronger” or “better” than another.
For an uncomplicated yeast infection, all are considered equally effective.
The primary difference is the concentration of the medication.
- 1-Day Treatment: This contains the highest concentration of medication in a single dose. It’s convenient but may cause more side effects like burning or irritation due to the high dose.
- 3-Day Treatment: This offers a balance between convenience and a lower concentration per dose.
- 7-Day Treatment: This uses the lowest concentration of medication, spread out over a week. It is often recommended for those with sensitive skin or who have experienced irritation from higher-dose treatments in the past.
Regardless of the regimen you choose, it may still take several days for symptoms to resolve completely.
You must complete the full course of treatment, even if you start to feel better, to ensure the infection is fully eradicated.
Pros and Cons of OTC Treatments
- Pros:
- Accessibility: Readily available at pharmacies and grocery stores without a prescription.
- Cost-Effective: Generally less expensive than a doctor’s visit and prescription medication.
- Convenience: Allows for immediate treatment without needing to schedule an appointment.
- Cons:
- Risk of Misdiagnosis: Studies show many women who self-treat for a yeast infection actually have another condition, like BV.
- Messiness: Creams and suppositories can be messy and may leak.
- Condom Compatibility: The oil-based formulas in many of these treatments can weaken latex condoms and diaphragms, increasing the risk of breakage and unintended pregnancy.
Which Prescription Medications Are Used for a Yeast Infection?
When an OTC treatment isn’t appropriate or has failed, a healthcare provider can offer more potent and targeted prescription options.
These are necessary for complicated, severe, or recurrent infections.
The Go-To Oral Antifungal: Fluconazole (Diflucan)
The most commonly prescribed treatment for a yeast infection is fluconazole, an oral antifungal medication sold under the brand name Diflucan.
For an uncomplicated infection, it is typically prescribed as a single 150 mg pill.
- Pros:
- Highly Effective: It works systemically (throughout the body) to clear the infection and is very effective.
- Convenience: A single pill is clean, simple, and far less messy than topical creams.
- Fast-Acting: While symptom relief isn’t instant, the medication begins working within 24 hours.
- Cons:
- Requires a Prescription: You must see a doctor to get it.
- Systemic Side Effects: Because it circulates in the bloodstream, it can cause side effects like headache, nausea, or abdominal pain, though these are uncommon.
- Drug Interactions: It can interact with other medications, so it’s vital to tell your doctor about everything you’re taking.
- Not for Pregnancy: Oral fluconazole is generally avoided during pregnancy due to a potential link with birth defects, especially at high doses. The CDC recommends only topical treatments for pregnant women.
Prescription-Strength Topical Treatments
In some cases, a doctor may prescribe a more potent topical antifungal than what’s available over the counter.
These are often used for infections caused by less common yeast species or for more severe inflammation. Examples include:
- Butoconazole (Gynazole-1)
- Terconazole (Terazol)
These medications come in cream or suppository form and offer a targeted approach for infections that may not respond to standard OTC options.
Newer Medications for Resistant or Recurrent Yeast
A significant advancement in treating yeast infections has been the development of new drugs for difficult cases.
These are reserved for recurrent or resistant infections, often caused by non-albicans species like Candida glabrata.
This demonstrates a deep understanding of the evolving landscape of fungal infections.
- Ibrexafungerp (Brexafemme): An oral medication from a new class of antifungals. It’s approved for treating VVC and reducing the incidence of RVVC.
- Oteseconazole (Vivjoa): Another newer oral antifungal specifically designed to prevent recurrent yeast infections in women who are not of reproductive potential.
These advanced options are prescribed by specialists and represent a crucial line of defense when standard therapies fail.
OTC vs. Prescription: A Head-to-Head Comparison
To help you visualize the key differences, here is a direct comparison between the most common OTC and prescription treatments.
| Feature | OTC Treatment (e.g., Miconazole) | Prescription Treatment (e.g., Fluconazole) |
|---|---|---|
| Form | Topical (Vaginal Cream, Suppository) | Oral (Pill) |
| Mechanism of Action | Acts locally on the surface of the vaginal tissue. | Acts systemically, circulating through the bloodstream. |
| Typical Use Case | Mild-to-moderate, uncomplicated infections in those who have been previously diagnosed. | First-time infections (for diagnosis), severe, complicated, or recurrent infections. |
| Effectiveness | Highly effective for uncomplicated infections caused by C. albicans. Studies show similar cure rates to oral fluconazole for simple cases. | Highly effective for both uncomplicated and complicated infections. The go-to for maintenance therapy. |
| Convenience | Can be messy, may require daily application for up to 7 days. | Clean and simple, often just a single dose. |
| Speed of Symptom Relief | External cream can provide immediate, temporary relief from itching. | Takes 24-48 hours for the medication to circulate and begin reducing symptoms from the inside out. |
| Accessibility | Available at any pharmacy without a prescription. | Requires a doctor’s visit and prescription. |
| Key Considerations | Oil-based creams can weaken latex condoms and diaphragms. Risk of misdiagnosis. | Potential for systemic side effects and drug interactions. Generally avoided during pregnancy. |
What If My Yeast Infection Keeps Coming Back?
For a small percentage of women, yeast infections are not an occasional nuisance but a chronic, frustrating problem.
If you experience three or more symptomatic yeast infections within a 12-month period, you have a condition known as Recurrent Vulvovaginal Candidiasis (RVVC).
This condition affects less than 5% of women but requires a more aggressive and structured treatment plan than a simple infection.
Managing RVVC is not about treating each infection as it comes; it’s about breaking the cycle.
The approach recommended by the Centers for Disease Control and Prevention (CDC) typically involves two phases:
- Induction Therapy: The first step is to achieve a complete cure of the current infection. This involves a longer course of initial treatment than for an uncomplicated infection. This might look like:
- 7-14 days of a topical azole cream or suppository.
- A multi-dose oral fluconazole regimen (e.g., one 150 mg pill every 72 hours for three doses).
- Maintenance Therapy: Once the initial infection is cleared, the goal is to prevent it from coming back. This is achieved with a long-term, suppressive medication regimen. The most common and well-studied maintenance therapy is:
- Weekly oral fluconazole (150 mg) for six months.
It’s also crucial to investigate potential underlying causes.
Your doctor may test for resistant yeast species, undiagnosed diabetes, or other immune-related issues that could be contributing to the recurrence.
How Is a “Complicated” Yeast Infection Treated?
A “complicated” yeast infection is one that involves severe symptoms, an unusual yeast species, or occurs in a host with specific health conditions.
These require specialized treatment beyond a single dose of fluconazole or a short course of OTC cream.
Treating Non-Albicans Candida
While Candida albicans causes most yeast infections, other species can be the culprit in 10-20% of cases, especially in recurrent infections.
The most common of these is Candida glabrata. This species is notoriously resistant to the standard azole antifungal drugs (like fluconazole and miconazole).
If a non-albicans species is identified via a vaginal culture, treatment must be adjusted. Options may include:
- Boric Acid Suppositories: A 600 mg boric acid capsule inserted vaginally once daily for 2-3 weeks is a common and effective treatment for azole-resistant yeast. It is important to note that boric acid is toxic if swallowed and should not be used during pregnancy.
- Other Antifungals: A doctor might prescribe other classes of antifungals, such as nystatin suppositories or flucytosine cream, sometimes in combination.
- Newer Oral Medications: As mentioned, ibrexafungerp and oteseconazole are effective against a broader range of Candida species.
Yeast Infection Treatment During Pregnancy
Hormonal changes during pregnancy make women more susceptible to yeast infections. However, treatment options are more limited due to safety concerns for the developing fetus.
The CDC and the American College of Obstetricians and Gynecologists (ACOG) are clear on this: only topical azole therapies, applied for a full 7 days, are recommended for use in pregnant women.
This means using a cream or suppository containing clotrimazole or miconazole.
Single-dose topical therapies and all oral antifungal pills (like fluconazole) are generally avoided due to a potential, though debated, risk of miscarriage and birth defects.
How to Tell the Difference: Yeast Infection vs. BV vs. UTI
One of the biggest challenges in vaginal health is that the symptoms of different conditions can overlap, leading to confusion and misdiagnosis.
The three most commonly confused conditions are yeast infections, Bacterial Vaginosis (BV), and Urinary Tract Infections (UTIs).
Understanding the key differences is vital, though a doctor’s diagnosis remains the gold standard.
Bacterial Vaginosis (BV) is caused by an overgrowth of certain bacteria in the vagina, disrupting the natural balance.
A Urinary Tract Infection (UTI) is a bacterial infection of the urinary system (bladder, urethra, kidneys).
This table breaks down the distinguishing features:
| Symptom / Feature | Yeast Infection | Bacterial Vaginosis (BV) | Urinary Tract Infection (UTI) |
|---|---|---|---|
| Primary Cause | Fungus (Candida albicans) | Bacteria (e.g., Gardnerella vaginalis) | Bacteria (e.g., E. coli) |
| Discharge Color & Consistency | Thick, white, clumpy (like cottage cheese) | Thin, watery, grayish-white | Not a primary vaginal symptom. Urine may be cloudy or bloody. |
| Discharge Odor | Typically odorless or may have a mild, yeasty smell. | Strong, unpleasant, “fishy” odor, especially after sex. | N/A (Urine may have a strong odor). |
| Main Sensation | Intense itching and burning of the vulva and vagina. | Mild itching or irritation. Often, odor is the main complaint. | Painful/burning urination, pelvic pain. |
| Location of Pain | Primarily vulva and vagina. | Primarily vagina. | Urethra, bladder, lower abdomen/pelvis. |
| Urination Symptoms | External burning as urine passes over inflamed, irritated skin. | Sometimes mild burning, but not a primary symptom. | Frequent, urgent need to pee; sharp, internal pain/stinging during urination. |
The most telling differences are often the odor and consistency of the discharge.
The fishy odor of BV and the cottage cheese-like discharge of a yeast infection are key differentiators.
The sharp, internal pain and urgency of urination are hallmarks of a UTI.
How Can I Prevent Future Yeast Infections?
While you can’t always prevent a yeast infection, adopting certain lifestyle and hygiene habits can significantly reduce your risk by helping to maintain a healthy, balanced vaginal environment.
- Wear Breathable Underwear: Cotton is the best choice as it allows air to circulate and doesn’t trap moisture. Avoid synthetic materials like nylon or spandex for daily wear.
- Keep Clothing Loose: Avoid wearing tight-fitting pants, leggings, or pantyhose for long periods, as they can trap heat and moisture, creating an ideal environment for yeast growth.
- Avoid Douching: Your vagina is self-cleaning. Douching disrupts the natural pH balance and washes away the beneficial bacteria that keep yeast in check.
- Steer Clear of Scented Products: Avoid scented tampons, pads, feminine sprays, and harsh soaps in the genital area. Clean the vulva with warm water only or a mild, unscented soap.
- Change Out of Wet Clothes Promptly: Don’t linger in a wet swimsuit or sweaty gym clothes. Change into dry clothes as soon as possible.
- Wipe from Front to Back: After using the toilet, always wipe from front to back to prevent bacteria from the anus from spreading to the vagina.
- Manage Your Blood Sugar: If you have diabetes, keeping your blood sugar levels under control is one of the most effective ways to prevent yeast infections.
- Use Antibiotics Wisely: Only take antibiotics when they are truly necessary and prescribed by a doctor. Never take them for a viral infection like a cold.
- Consider Probiotics: While scientific evidence is still emerging and not conclusive, some studies suggest that consuming yogurt with live cultures or taking a probiotic supplement containing Lactobacillus strains may help maintain a healthy vaginal microbiome. This should be seen as a supportive measure, not a primary treatment or prevention strategy. Some women find this helpful, but it’s not a guaranteed solution.
Frequently Asked Questions (FAQ)
1. Can a yeast infection go away on its own?
It is highly unlikely. While very mild cases might resolve, most yeast infections require antifungal medication to clear the overgrowth of Candida. Without treatment, symptoms are likely to persist or worsen, so it’s always best to seek treatment.
2. How long does it take for a yeast infection to clear up with treatment?
With proper treatment, most uncomplicated yeast infections begin to improve within a few days, with complete resolution in about a week. It’s crucial to complete the full course of medication, even if you feel better, to prevent recurrence.
3. Can men get yeast infections?
Yes, men can get a yeast infection on the penis, a condition called balanitis. It can cause redness, itching, and a burning sensation on the head of the penis. It is often treated with a topical antifungal cream.
4. Should I have sex if I have a yeast infection?
It’;s best to avoid sexual intercourse until the infection has completely cleared. Sex can worsen irritation and inflammation, delay healing, and potentially spread the infection to your partner. Additionally, oil-based creams can damage latex condoms.
5. Does eating yogurt cure a yeast infection?
No, eating yogurt is not a cure for an active yeast infection. While yogurt with live probiotic cultures can help support a healthy vaginal microbiome as a preventive measure, it does not contain the antifungal properties needed to eliminate an established infection.
6. What is the fastest way to get rid of a yeast infection?
The fastest way to get relief is to use an effective antifungal treatment. A single-dose oral pill like fluconazole is very convenient, while topical creams can provide faster relief for external itching. The “fastest” option depends on getting the right diagnosis and treatment promptly.
7. Can stress cause a yeast infection?
While stress itself doesn’t directly cause a yeast infection, chronic stress can weaken the immune system. A suppressed immune system may be less effective at keeping Candida levels in check, potentially making you more susceptible to an infection.
8. Is it safe to use an OTC treatment if I’m not 100% sure it’s a yeast infection?
No, it’s not recommended. Using an antifungal when you actually have a bacterial infection like BV can make the underlying problem worse and delay proper treatment. If you have any doubt, it is always safest to see a healthcare provider for an accurate diagnosis.
Conclusion
Navigating the discomfort of a yeast infection can be frustrating, but understanding your options is empowering.
We’ve seen that the key to effective treatment lies in recognizing the difference between an uncomplicated infection, which can often be managed with accessible OTC products, and a complicated or recurrent infection that demands a professional diagnosis and prescription care.
Both over-the-counter topical creams and prescription oral pills are highly effective when used correctly for the right situation.
The most critical takeaway is the importance of an accurate diagnosis.
Self-treating can be risky if you’re not certain about the cause of your symptoms, especially if it’s your first time or if infections keep returning.
Ultimately, you are the best advocate for your own health. By arming yourself with this knowledge, you can make confident, informed decisions.
If you are in doubt, experiencing severe symptoms, or dealing with the frustration of recurrent infections, the most important step you can take is to consult a healthcare provider.
They can provide a definitive diagnosis and create a treatment plan tailored specifically to your needs, setting you on the fastest path to relief and long-term wellness.
Reference
[1] Vaginal Yeast Infection: Causes, Symptoms & Treatment
https://my.clevelandclinic.org/health/diseases/5019-vaginal-yeast-infection
[2] Vulvovaginal Candidiasis – STI Treatment Guidelines
https://www.cdc.gov/std/treatment-guidelines/candidiasis.htm
[3] Candidiasis (yeast infection)
https://www.who.int/news-room/fact-sheets/detail/candidiasis-(yeast-infection)
[4] Preventing Vaginal Yeast Infections With Lifestyle and Diet …
[5] Treatment of Vulvovaginal Candidiasis—An Overview of Guidelines …
https://pmc.ncbi.nlm.nih.gov/articles/PMC10455317
[6] Comparing Common Vaginal Health Issues – Momotaro Apotheca
[7] Bacterial Vaginosis vs Yeast Infection: What’s the Difference?
https://khealth.com/learn/yeast-infection/vs-bacterial-vaginosis
[8] Yeast Infection Treatment Guide – OTC, Prescription & …
[9] Treatment of Candidiasis – CDC

