Overcoming daily fatigue involves identifying its root cause—whether it’s lifestyle habits, an underlying medical condition, or mental health strain—and implementing targeted, evidence-based strategies.
This isn’t about a quick fix, it’s about understanding the complex signals your body is sending and responding with precision and care.
If you feel perpetually drained, you are far from alone.
According to a recent report from the Centers for Disease Control and Prevention (CDC), over 13% of U.S. adults report feeling very tired or exhausted most days or every day.
This pervasive sense of exhaustion goes beyond simple sleepiness.
It’s crucial to understand the difference: tiredness is a normal, expected response to physical or mental exertion that is resolved by rest.
Fatigue, on the other hand, is a profound, persistent, and often debilitating lack of energy that rest doesn’t seem to touch.
It’s a state of exhaustion that can interfere with your daily life, work, and well-being.
This guide is designed to be your definitive resource for navigating the complexities of fatigue.
We will explore how to pinpoint the specific causes of your exhaustion, from common lifestyle factors to more complex medical conditions.
You’ll discover actionable, science-backed strategies for an immediate energy boost, take a deep dive into misunderstood conditions like Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), and learn exactly when it’s time to seek professional medical help.
Continue reading to start your journey from exhausted to energized.
In This Article
What Causes Fatigue? Uncovering the Root of Your Exhaustion
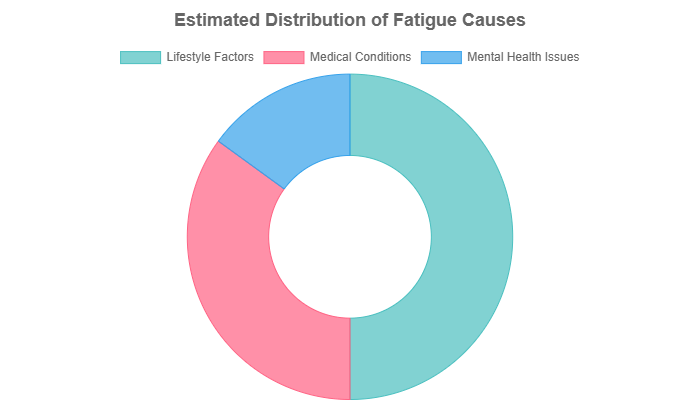
Fatigue is rarely caused by a single factor. More often, it’s a complex interplay of lifestyle choices, physical health, and mental well-being.
Think of your energy as a bank account, various factors can either make deposits or withdrawals. Identifying the primary sources of your energy drain is the first and most critical step toward reclaiming your vitality.
The causes of fatigue can be broadly categorized into three main areas, as illustrated below.
Is Your Lifestyle Draining Your Energy?
For many people, persistent fatigue is a direct result of daily habits.
While these factors may seem obvious, their cumulative impact can be profound.
It’s essential to honestly assess these areas of your life, as they are often the most accessible to change and can yield significant improvements in energy levels.
The Sleep-Fatigue Connection
It’s not just about the number of hours you sleep, it’s about the quality of that sleep.
You can spend eight hours in bed and still wake up feeling unrefreshed if your sleep is fragmented or non-restorative.
Poor sleep hygiene—such as inconsistent bedtimes, exposure to blue light from screens before bed, or an uncomfortable sleep environment—can sabotage sleep quality.
Furthermore, undiagnosed sleep disorders like sleep apnea, where breathing repeatedly stops and starts, can lead to severe daytime fatigue despite adequate time in bed.
How Your Diet Dictates Your Energy
The food you eat is the fuel your body runs on.
A diet high in processed foods, sugar, and refined carbohydrates can lead to rapid blood sugar spikes followed by dramatic crashes, leaving you feeling sluggish and irritable.
Nutrient deficiencies are another major culprit. Low levels of iron, vitamin B12, or vitamin D are strongly linked to fatigue.
Dehydration is also a surprisingly common cause, even mild dehydration can impair cognitive function and lead to feelings of exhaustion.
The Exercise Paradox: Too Much or Too Little?
Exercise presents a paradox when it comes to fatigue.
A sedentary lifestyle leads to deconditioning, where your body becomes less efficient at using energy, making even small tasks feel tiring.
On the other hand, overtraining syndrome, common in athletes or highly active individuals who don’t allow for adequate recovery, can cause deep, persistent fatigue, mood disturbances, and decreased performance.
The key is finding a sustainable balance of regular, moderate activity.
The Hidden Energy Sappers: Stress, Alcohol, and Caffeine
Chronic stress keeps your body in a constant state of “fight or flight”, flooding it with hormones like cortisol.
This sustained state of high alert is incredibly draining on your physical and mental resources.
Alcohol, while it may help you fall asleep initially, severely disrupts the later, more restorative stages of sleep, leading to a net loss in sleep quality.
Caffeine is a temporary loan of energy, relying on it can create a boom-and-bust cycle that masks underlying exhaustion and disrupts natural sleep patterns, ultimately worsening your overall fatigue.
Could a Medical Condition Be the Cause of Your Fatigue?
When lifestyle adjustments don’t resolve your fatigue, it’s crucial to consider an underlying medical cause.
Fatigue is one of the most common symptoms across a vast range of illnesses, acting as a check-engine light for your body.
A thorough medical evaluation is essential to rule out or diagnose these conditions.
Common Culprits Your Doctor Will Check First
- Anemia: Particularly iron-deficiency anemia, this condition means you have fewer red blood cells or less hemoglobin to carry oxygen to your tissues. Without adequate oxygen, your body can’t produce energy efficiently, leading to classic symptoms of fatigue, weakness, and shortness of breath.
- Thyroid Disorders: The thyroid gland is the master regulator of your metabolism. Hypothyroidism (an underactive thyroid) slows everything down, causing profound fatigue, weight gain, and cold intolerance. Conversely, hyperthyroidism (an overactive thyroid) puts your body into overdrive, which can also lead to exhaustion and burnout.
- Diabetes: In both Type 1 and Type 2 diabetes, problems with insulin and glucose regulation mean your cells aren’t getting the sugar they need for energy. This cellular energy crisis manifests as persistent and often overwhelming fatigue.
Inflammatory and Autoimmune Conditions
In conditions like Rheumatoid Arthritis, Lupus, or Inflammatory Bowel Disease (IBD), the immune system mistakenly attacks the body’s own tissues.
This triggers chronic, systemic inflammation.
The constant immune response consumes a massive amount of energy and releases inflammatory proteins called cytokines, which are known to induce feelings of fatigue and malaise, similar to how you feel when you have the flu.
Heart and Lung Conditions
Your heart and lungs work together to deliver oxygen-rich blood to your entire body.
Any condition that impairs this process will inevitably cause fatigue. In Chronic Obstructive Pulmonary Disease (COPD), damaged lungs struggle to take in enough oxygen.
In conditions like Congestive Heart Failure, a weakened heart can’t pump blood efficiently. In both cases, the body is starved of the oxygen it needs for basic energy production.
How Does Mental Health Affect Your Physical Energy?
The connection between mind and body is powerful and undeniable.
Mental health conditions are not “all in your head”, they have profound physiological consequences that can drain your physical energy reserves just as surely as a medical illness.
The Weight of Depression and Anxiety
Depression is more than just sadness, it involves significant changes in brain chemistry that affect sleep, appetite, and motivation, all of which are cornerstones of energy.
The anhedonia (loss of pleasure) associated with depression can make even enjoyable activities feel like a chore.
Anxiety, with its state of constant hypervigilance and worry, is like leaving a car’s engine running 24/7.
This sustained mental and physiological arousal is incredibly exhausting and is a primary driver of physical fatigue.
Understanding Burnout and Emotional Exhaustion
While not a formal medical diagnosis in the same way as depression, burnout is a recognized state of emotional, physical, and mental exhaustion caused by prolonged or excessive stress.
It’s often tied to one’s job but can also result from other long-term stressors, such as caregiving.
Burnout is characterized by feelings of energy depletion, increased mental distance from one’s job or responsibilities, and reduced professional efficacy.
It represents a specific type of fatigue born from a mismatch between demands and resources in a particular area of life.
How to Fight Fatigue: Evidence-Based Strategies for More Energy
Once you have a better understanding of what might be causing your fatigue, you can begin to implement targeted, evidence-based strategies.
The following recommendations are foundational pillars for building and sustaining energy.
Focus on incorporating them gradually and consistently for the best results.
How Can You Optimize Your Sleep for Maximum Energy?
Improving sleep is often the single most effective strategy for combating fatigue.
This goes beyond simply trying to sleep more, it involves creating the right conditions for deep, restorative sleep.
Adopt the following sleep hygiene protocol to transform your nights and energize your days.
- Maintain a Consistent Sleep-Wake Cycle: Go to bed and wake up at the same time every day, even on weekends. This reinforces your body’s natural circadian rhythm, making it easier to fall asleep and wake up feeling refreshed.
- Create a “Wind-Down” Routine: In the hour before bed, engage in relaxing activities. This could include reading a physical book, listening to calm music, gentle stretching, or taking a warm bath. This signals to your brain that it’s time to prepare for sleep.
- Optimize Your Bedroom Environment: Your bedroom should be a sanctuary for sleep. Keep it cool, dark, and quiet. Use blackout curtains, an eye mask, and earplugs or a white noise machine if necessary.
- Limit Blue Light Exposure Before Bed: The blue light emitted by phones, tablets, and computers suppresses the production of melatonin, the hormone that regulates sleep. Avoid screens for at least an hour before bedtime.
- Practice Strategic Napping: If you need to nap, keep it short (20-30 minutes) and do it in the early afternoon. Long or late-afternoon naps can interfere with nighttime sleep and worsen fatigue in the long run.
What Should You Eat to Combat Fatigue?
Your diet provides the raw materials for energy production.
An anti-fatigue diet focuses on stable blood sugar, nutrient density, and proper hydration.
Building an Anti-Fatigue Plate
To avoid energy-draining blood sugar rollercoasters, build your meals around a combination of complex carbohydrates, lean proteins, and healthy fats.
Complex carbs (like whole grains, legumes, and vegetables) provide a slow, steady release of energy.
Protein and fat help slow the absorption of carbohydrates, further promoting stable energy levels and increasing satiety.
The Importance of Micronutrients
Certain vitamins and minerals play a direct role in energy metabolism. Ensure your diet is rich in these key nutrients:
- Iron: Essential for creating hemoglobin, which carries oxygen. Found in lean red meat, poultry, fish, lentils, spinach, and fortified cereals.
- B Vitamins (especially B12): Crucial for converting food into usable energy. Found in meat, fish, eggs, dairy, and nutritional yeast.
- Magnesium: Involved in hundreds of biochemical reactions in the body, including energy production. Found in nuts, seeds, leafy greens, and dark chocolate.
Hydration as an Energy Multiplier
Dehydration is a common and often overlooked cause of fatigue.
When you’re dehydrated, your blood volume decreases, forcing your heart to work harder to pump blood to your muscles and organs.
This extra effort leads to exhaustion.
Aim to drink water consistently throughout the day, not just when you feel thirsty.
A general guideline is to drink at least eight 8-ounce glasses, but your needs may be higher depending on your activity level and climate.
What is the Best Way to Exercise for More Energy?
While it may seem counterintuitive, expending energy through exercise is one of the most effective ways to generate more energy.
The key is to approach it correctly.
A landmark 2022 meta-analysis published in the Psychology of Sport and Exercise journal synthesized data from dozens of studies and found that chronic exercise significantly reduces feelings of fatigue and increases feelings of energy and vitality.
The research highlights that moderate-intensity exercise provides the most consistent benefits.
Furthermore, interventions that combined aerobic exercise (like brisk walking, cycling, or swimming) with resistance training (like lifting weights or using resistance bands) were significantly more beneficial for boosting energy than aerobic exercise alone.
For beginners, it’s crucial to start slow to avoid triggering more exhaustion. Consider this sample weekly plan:
- Monday & Thursday: 20-30 minutes of moderate aerobic activity (e.g., brisk walk where you can still hold a conversation).
- Tuesday & Friday: 15-20 minutes of simple resistance training (e.g., bodyweight squats, push-ups against a wall, lunges).
- Wednesday, Saturday, Sunday: Active rest (e.g., gentle stretching, a leisurely walk).
How Can You Manage Stress to Preserve Your Energy?
Chronic stress is a major energy thief. Learning to manage your stress response can free up significant mental and physical resources, directly combating fatigue.
Mindfulness and Meditation
Practices like mindfulness and meditation train your brain to step back from the constant stream of stressful thoughts.
This helps lower the production of the stress hormone cortisol and reduces the mental chatter that contributes to exhaustion.
Even 5-10 minutes of daily guided meditation can have a noticeable impact on your energy and resilience.
The Power of Pacing
Pacing is a crucial energy management technique that involves consciously balancing activity with strategic rest.
Instead of pushing yourself to the point of exhaustion and then crashing, you learn to listen to your body’s signals and take breaks before you become depleted.
This proactive approach helps you stay within your “energy envelope”, preventing the boom-and-bust cycles that perpetuate fatigue.
We will explore this concept in more detail later, as it is the cornerstone of managing complex fatigue conditions.
Deeper Dive: When Fatigue is a Complex Medical Puzzle
Sometimes, fatigue isn’t just a matter of lifestyle adjustments.
It can be the primary symptom of a complex, chronic illness that is often misunderstood by the public and even by some medical professionals.
This section delves into these challenging conditions, armed with the latest scientific research, to provide clarity and debunk harmful myths.
What is Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)?
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a severe, long-term, and debilitating multi-system disease.
It is far more than being “chronically tired“.
It’s a state of pathological exhaustion that can leave individuals housebound or even bedbound, dramatically reducing their quality of life.
Beyond Tiredness: The Defining Symptoms
The absolute hallmark symptom of ME/CFS is Post-Exertional Malaise (PEM).
This is a severe worsening of all symptoms after even minimal physical, mental, or emotional exertion.
The crash can be delayed by hours or even days and can last for days, weeks, or longer. Other core symptoms include:
- Unrefreshing Sleep: Waking up feeling just as tired, or even more so, than when you went to bed.
- Cognitive Impairment: Often referred to as “brain fog”, this includes problems with memory, concentration, and information processing.
- Orthostatic Intolerance: Symptoms (like dizziness, palpitations, and fatigue) worsen when standing or sitting upright and are relieved by lying down.
The Latest Science: What Researchers Are Discovering
For decades, ME/CFS patients have struggled with medical dismissal.
However, recent, rigorous research is finally uncovering the biological underpinnings of the disease.
A groundbreaking in-depth study from the National Institutes of Health (NIH), published in February 2024 in Nature Communications, provided significant new clues.
“This in-depth study of a small group of people found a number of factors that likely contribute to their ME/CFS. Now researchers can test whether these findings apply to a larger patient group and move towards identifying treatments that target core drivers of the disease.” — Walter Koroshetz, M.D., NINDS Director
The study revealed several key abnormalities in ME/CFS patients compared to healthy controls:
- Brain Abnormalities: Researchers found reduced activity in a brain region called the temporal-parietal junction (TPJ), which is involved in processing how the brain decides to exert effort. This suggests the fatigue in ME/CFS may be a brain-based disorder of effort perception, not a lack of motivation.
- Immune System Dysregulation: The study identified distinct differences in immune cells, particularly B cells, suggesting the immune system remains chronically activated after an initial infection.
- Metabolic Changes: Analysis of spinal fluid showed abnormally low levels of certain neurochemicals (catecholamines) that regulate the nervous system, linking brain imbalances directly to physical and cognitive symptoms.
Why Graded Exercise is Harmful and Pacing is Essential
Based on flawed past research, some doctors used to recommend Graded Exercise Therapy (GET) for ME/CFS, which involves progressively increasing physical activity.
However, due to the central nature of PEM, this approach is now widely understood to be inappropriate and potentially harmful for ME/CFS patients, often leading to severe and lasting relapses.
As the American Academy of Family Physicians now clarifies, exercise is no longer recommended.
The current, evidence-based management strategy is pacing.
The “Stop, Rest, Pace” approach teaches patients to recognize their limited energy envelope and to stay within it, using strategic rest to avoid triggering PEM.
Is “Adrenal Fatigue” Real? The Scientific Truth
The term “adrenal fatigue” is widely used in alternative medicine circles to describe a collection of symptoms including exhaustion, brain fog, body aches, and sleep disturbances, supposedly caused by overworked adrenal glands from chronic stress.
It’s crucial to state this clearly: your symptoms are real and valid, but “adrenal fatigue” is not the cause.
Acknowledging the Symptoms, Questioning the Label
If you’ve been told you have “adrenal fatigue”, it’s likely because you are experiencing very real and distressing symptoms.
The feeling of being completely depleted by stress is a legitimate experience.
However, attributing these symptoms to a non-existent condition can prevent you from finding the true cause and getting effective treatment.
What the Science Says
Major medical and scientific bodies are in agreement: “adrenal fatigue” is not a recognized medical diagnosis.
The Endocrine Society, the world’s leading organization for hormone research and clinical endocrinology, has stated there is no scientific proof to support it.
A systematic review of 58 studies concluded that there is “no substantiation that ‘adrenal fatigue’ is an actual medical condition”.
The theory posits that your adrenal glands “burn out”, but there is no evidence this happens outside of recognized adrenal diseases like Addison’s disease (adrenal insufficiency), which is a serious, diagnosable condition with specific biomarkers.
What Might Really Be Happening?
So, if it’s not “adrenal fatigue”, what is causing your symptoms? The answer likely lies in scientifically accepted concepts:
- HPA Axis Dysfunction: Chronic stress can disrupt the communication between your hypothalamus, pituitary gland, and adrenal glands (the HPA axis). This doesn’t mean your adrenals are “fatigued”, but that the entire stress-response system is dysregulated, which can certainly cause fatigue and other related symptoms.
- Undiagnosed Medical Conditions: The symptoms attributed to “adrenal fatigue” overlap significantly with those of hypothyroidism, anemia, sleep apnea, depression, and ME/CFS.
- Lifestyle Factors: The cumulative effect of poor sleep, a nutrient-poor diet, and chronic stress can produce the exact constellation of symptoms labeled as “adrenal fatigue”.
The most important step is to work with a qualified healthcare professional to get an accurate diagnosis rather than self-treating a debunked term.
How Do Different Types of Fatigue Compare?
Understanding the nuances between different fatigue states can help you better communicate your experience to a doctor and guide you toward the right solutions.
The table below compares three common, yet distinct, forms of profound exhaustion.
| Feature | General Fatigue | Burnout | ME/CFS |
|---|---|---|---|
| Primary Cause | Lifestyle factors (poor sleep, diet, stress), acute illness, or side effect of a medical condition. | Chronic, unmanaged stress related to a specific domain (usually work or caregiving). | A complex, multi-system neuroimmune disease, often triggered by an infection. |
| Key Symptom | A feeling of tiredness, weariness, or lack of energy that is generally proportional to exertion. | Emotional exhaustion, cynicism/detachment from the stressor, and a sense of ineffectiveness. | Post-Exertional Malaise (PEM): a severe worsening of all symptoms after minimal exertion. |
| Effect of Rest | Rest and sleep are generally restorative and relieve the fatigue. | Rest provides temporary relief, but fatigue returns quickly upon re-engaging with the stressor. A long break (e.g., vacation) is often needed. | Sleep is typically unrefreshing. Rest is necessary but does not resolve the underlying fatigue. Pushing through leads to PEM. |
| Recommended Approach | Improve sleep hygiene, diet, and exercise. Address any underlying medical issues. | Address the source of stress, set boundaries, take time off, and seek support (e.g., therapy, coaching). | Pacing (“Stop, Rest, Pace”) to stay within the energy envelope, symptom management, and medical support. Avoid overexertion. |
Your Action Plan: When and How to See a Doctor
While lifestyle changes are powerful, they are not a substitute for professional medical care.
If your fatigue is persistent, severe, or accompanied by other concerning symptoms, a visit to your doctor is essential.
Proper diagnosis is the key to effective treatment.
What Are the Red Flag Symptoms That Require a Doctor’s Visit?
Don’t dismiss persistent fatigue. Make an appointment with your healthcare provider if you experience any of the following:
- Your fatigue has lasted for two weeks or more despite making positive changes to your sleep, diet, and stress levels.
- Your fatigue is accompanied by unexplained weight loss or gain.
- You have other systemic symptoms like a persistent low-grade fever, night sweats, or swollen lymph nodes.
- You experience alarming symptoms such as a severe headache, chest pain, shortness of breath, or feelings of faintness. (These may require immediate medical attention).
- Your fatigue is associated with symptoms of depression, anxiety, or thoughts of self-harm. (Please seek help immediately).
- The fatigue is so severe that it significantly interferes with your ability to work, socialize, or perform daily activities.
How Can You Prepare for Your Doctor’s Appointment?
To make your visit as productive as possible, come prepared.
Doctors have limited time, and providing clear, organized information can help them pinpoint the cause of your fatigue more effectively.
Before your appointment, start a “fatigue journal”.
In your journal, track the following for at least a week:
- Timing and Onset: When did the fatigue start? Was it sudden or gradual? Is it worse at certain times of the day?
- Severity: On a scale of 1 to 10 (with 10 being the most severe exhaustion you can imagine), how would you rate your fatigue each day?
- Triggers and Relievers: What makes your fatigue worse (e.g., physical activity, stress, certain foods)? What, if anything, makes it better?
- Associated Symptoms: Note any other symptoms you’re experiencing, even if they seem unrelated (e.g., pain, digestive issues, brain fog, dizziness).
- Medications and Supplements: Make a complete list of every medication, vitamin, and supplement you take, including dosages.
During your appointment, you can expect your doctor to take a detailed history, perform a physical exam, and likely order some initial blood tests.
Common tests include a Complete Blood Count (CBC) to check for anemia, a thyroid panel (TSH), blood glucose levels to check for diabetes, and tests for vitamin deficiencies.
Frequently Asked Questions (FAQ) About Fatigue
Can vitamin deficiencies cause severe fatigue?
Yes, absolutely. Deficiencies in key nutrients like iron, vitamin B12, and vitamin D are well-established causes of significant fatigue. These vitamins are crucial for red blood cell production, oxygen transport, and energy metabolism. A simple blood test can identify these deficiencies.
What’s the difference between chronic fatigue and Chronic Fatigue Syndrome?
Chronic fatigue is a symptom—fatigue lasting more than six months. Chronic Fatigue Syndrome (ME/CFS) is a specific, complex disease where chronic fatigue is a core symptom, but it must be accompanied by others, most importantly post-exertional malaise (PEM).
Why do I feel tired even after 8 hours of sleep?
This points to poor sleep quality rather than quantity. It could be caused by a sleep disorder like sleep apnea, frequent awakenings you don’t remember, or an underlying medical condition. It’s a key sign that your sleep is not restorative.
Can stress alone cause physical fatigue?
Yes. Chronic stress keeps your body in a state of high alert (the “fight or flight” response), which consumes enormous amounts of energy. The constant production of stress hormones and the mental load of worry are physically exhausting over time.
Is it better to rest or exercise when you feel fatigued?
It depends on the cause. For general fatigue from a sedentary lifestyle, gentle, moderate exercise can actually boost energy. For fatigue from ME/CFS, exercise can be harmful and trigger a crash (PEM). In that case, pacing and strategic rest are essential.
How long does it take to recover from burnout-related fatigue?
Recovery from burnout is not quick and requires significant changes. It often takes months and involves addressing the root cause of the stress, taking substantial time off to rest, and developing new coping strategies and boundaries to prevent recurrence.
Can gut health affect my energy levels?
Yes, emerging research shows a strong link. An unhealthy gut microbiome can lead to inflammation, poor nutrient absorption, and affect the production of neurotransmitters, all of which can contribute to feelings of fatigue and low mood.
What is the first step to take if I have unexplained fatigue?
The first step is to honestly evaluate your lifestyle: sleep, diet, exercise, and stress. If you make improvements in these areas for a couple of weeks and see no change, the next and most important step is to schedule an appointment with your doctor.
Conclusion
Fatigue is more than just a feeling, it’s a complex and important signal from your body that something is out of balance.
As we’ve explored, the path to recovery is not a one-size-fits-all solution but a personalized journey of investigation and action.
The journey begins with a three-pronged approach: first, building a strong foundation by optimizing the pillars of lifestyle—sleep, nutrition, movement, and stress management.
Second, courageously investigating potential medical causes with a qualified healthcare professional, refusing to accept “you’re just tired” as an answer.
And third, practicing self-compassion and embracing the crucial concept of energy management, or pacing, especially when dealing with complex chronic conditions.
Feeling perpetually exhausted can feel hopeless, but knowledge is power, and action is the antidote.
You now have a comprehensive map to guide you. Your journey to renewed energy starts now.
Choose one small, concrete step from this guide today—whether it’s scheduling that long-overdue doctor’s appointment, planning a 15-minute walk after lunch, or committing to a screen-free hour before bed—and do it.
That single step is the beginning of reclaiming not just your energy, but your life.
We invite you to share your experiences, questions, or your own successful strategies for overcoming fatigue in the comments section below. Your story could be the spark of hope for someone else on this journey.
Medical Disclaimer
The information provided in this article is for educational and informational purposes only and is not intended as medical advice. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.

