If you’ve ever felt like your brain is running on low battery—struggling to focus, remember simple things, or think clearly—you’ve likely experienced brain fog.
It’s not a medical diagnosis itself, but a collection of symptoms that can be frustrating and debilitating. And you’re not alone.
A large-scale 2024 study revealed that a staggering 28.2% of people report experiencing brain fog, highlighting it as a significant public health concern (PubMed Central).
This comprehensive guide will demystify brain fog.
We’ll explore its common symptoms, delve into the wide range of potential causes—from lifestyle habits to complex medical conditions like Long COVID—and provide evidence-based, actionable strategies to help you clear the haze and reclaim your mental clarity.
In This Article
What Exactly Is Brain Fog? (And What It Feels Like)
Brain fog isn’t about having a single “off” day.
It’s a persistent state of mental cloudiness that impairs your cognitive function.
People often describe it as feeling like their brain is “stuck in first gear”, “wrapped in cotton” or constantly buffering like a slow internet connection.
While the experience is subjective, it consistently involves a noticeable decline in your ability to think, process information, and concentrate.
Medically, brain fog is often referred to as cognitive dysfunction. It represents a cluster of symptoms rather than a standalone disease. It affects your executive functions—the mental skills that include working memory, flexible thinking, and self-control.
Unlike the gradual cognitive decline associated with aging or the severe confusion of delirium, brain fog is often characterized by a frustrating awareness that your mind isn’t working as it should be.
You know you’re capable of more, but something is holding you back, making even simple daily tasks feel like a monumental effort.
Key Symptoms of Brain Fog
Brain fog manifests differently for everyone, but certain symptoms are nearly universal.
Recognizing them is the first step toward identifying the cause and finding a solution. Here are the most common signs:
- Difficulty Concentrating: You can’t focus on a task, conversation, or even a TV show for an extended period. Your mind wanders easily.
- Short-Term Memory Problems: You frequently forget why you walked into a room, misplace keys, or can’t recall information you just heard or read.
- Slowed Thinking: Processing information, solving problems, or making decisions takes much longer than usual. You feel mentally sluggish.
- Mental Fatigue: Thinking itself feels exhausting. Even minor mental effort can leave you feeling drained.
- Trouble with Word-Finding: You struggle to find the right words during conversations, often feeling like the word is on the “tip of your tongue”.
- Feeling Disoriented or “Spaced Out”: A general sense of confusion or detachment from your surroundings.
- Difficulty Multitasking: Juggling multiple tasks, which you might have handled easily before, now feels overwhelming.
The Root Causes: Why Am I Experiencing Brain Fog?
Brain fog is a symptom, not the root problem. It’s your body’s signal that something is out of balance.
The causes are incredibly varied and often interconnected, ranging from simple lifestyle factors to complex medical issues.
Lifestyle Factors
- Chronic Stress: Prolonged stress elevates cortisol levels, which can exhaust the brain, impair memory, and disrupt neurotransmitter function.
- Sleep Deprivation: Sleep is crucial for the brain’s glymphatic system to clear out toxins. A lack of quality sleep prevents this “housekeeping”, leading to cognitive impairment.
- Poor Diet: A diet high in processed foods, sugar, and unhealthy fats can promote inflammation and oxidative stress, both of which are enemies of brain health. Nutrient deficiencies, especially in B vitamins, iron, and omega-3s, are also major culprits.
- Dehydration: Even mild dehydration can reduce concentration and affect memory and other cognitive functions.
- Lack of Physical Activity: Exercise increases blood flow to the brain, promotes the growth of new neurons, and reduces inflammation. A sedentary lifestyle does the opposite.
Underlying Medical Conditions
Persistent brain fog is often linked to an underlying health condition, many of which involve systemic inflammation.
- Long COVID & Post-Viral Syndromes: As we’ll explore further, viruses like SARS-CoV-2 can trigger persistent neuroinflammation.
- Autoimmune Diseases: Conditions like Multiple Sclerosis (MS), Lupus, Rheumatoid Arthritis, and Hashimoto’s thyroiditis involve the immune system mistakenly attacking the body, causing widespread inflammation that can affect the brain.
- Hormonal Imbalances: Fluctuations during menopause (“meno-fog”), pregnancy, or due to thyroid disorders (hypothyroidism) can significantly impact cognitive function.
- Mental Health Conditions: Depression and anxiety are strongly linked to brain fog. They can affect neurotransmitter levels, disrupt sleep, and increase stress hormones, all contributing to cognitive difficulties.
- Chronic Fatigue Syndrome (CFS/ME) & Fibromyalgia: These conditions are characterized by profound fatigue and pain, with “fibro fog” being a hallmark symptom.
- Gut Health Issues: The gut-brain axis is a critical communication pathway. Conditions like Celiac disease or Inflammatory Bowel Disease (IBD) can lead to nutrient malabsorption and inflammation that travels to the brain.
Medications and Medical Treatments
Sometimes, the treatment is the cause. Certain medications are known to cause brain fog as a side effect, including some antidepressants, antihistamines, blood pressure medications, and sleep aids.
Chemotherapy is so notorious for this that the resulting cognitive impairment has its own name: “chemo brain”.
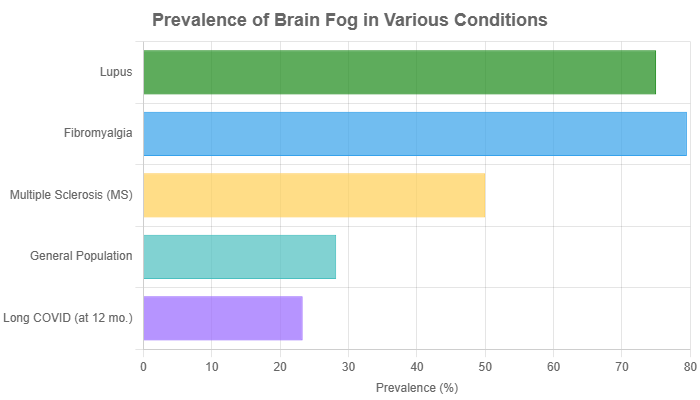
Data sourced from studies published in PubMed Central, ScienceDirect, and other medical reports. Prevalence in some conditions like Fibromyalgia and Lupus reflects “subjective cognitive symptoms”.
The Long COVID Connection: A Deep Dive into Post-Viral Brain Fog
One of the most discussed causes of brain fog today is Long COVID.
Research shows that a significant portion of people who recover from COVID-19 experience lingering cognitive issues.
A 2024 meta-analysis found the prevalence of brain fog at 12 months post-infection to be 23.3% (ScienceDirect).
Scientists are uncovering several mechanisms behind this phenomenon:
- Neuroinflammation: The virus can trigger a persistent inflammatory response in the brain. Immune cells called microglia become over-activated, releasing inflammatory molecules (cytokines) that disrupt normal neuronal function.
- Blood-Brain Barrier Disruption: Groundbreaking research in 2024 showed that Long COVID brain fog is associated with a “leaky” blood-brain barrier, allowing inflammatory substances from the blood to enter the brain (Nature Neuroscience).
- Reduced Blood Flow: Some studies suggest reduced blood flow to certain brain regions, starving them of oxygen and nutrients.
- Gut-Brain Axis Disruption: The virus can alter the gut microbiome, which may reduce the production of key neurotransmitters like serotonin, impacting mood and cognition (Cleveland Clinic).
How to Get Rid of Brain Fog: A 5-Step Strategic Plan
Clearing brain fog requires a holistic approach that addresses its root causes.
While you should always consult a doctor to rule out underlying conditions, these five evidence-based strategies can make a significant difference.
Step 1: Optimize Your Diet for Mental Clarity
Your brain consumes about 20% of your body’s energy, so what you eat directly impacts its function.
Adopt an anti-inflammatory eating pattern, such as the Mediterranean diet.
- Foods to Emphasize:
- Omega-3 Fatty Acids: Found in fatty fish (salmon, mackerel), walnuts, and flaxseeds. They are crucial for building brain cells and reducing inflammation.
- Antioxidant-Rich Foods: Berries, dark leafy greens (spinach, kale), and colorful vegetables fight oxidative stress.
- Lean Proteins: Chicken, beans, and lentils provide amino acids, the building blocks for neurotransmitters.
- Complex Carbohydrates: Whole grains, quinoa, and sweet potatoes provide a steady supply of glucose for brain energy.
- Foods to Limit:
- Sugar and Refined Carbs: Cause energy spikes and crashes and promote inflammation.
- Processed Foods and Unhealthy Fats: Can impair memory and increase oxidative stress.
Step 2: Strategic Supplementation (What the Evidence Shows)
While a food-first approach is best, certain supplements may help fill nutritional gaps and support cognitive function.
Always consult with a healthcare provider before starting any new supplement.
| Supplement | Potential Benefit for Brain Fog | Scientific Backing & Source |
|---|---|---|
| Omega-3 (DHA/EPA) | Reduces neuroinflammation, supports brain cell structure, and may improve memory and mood. | Multiple studies show a link between omega-3 intake and better cognitive function. (PMC/NCBI) |
| Vitamin D | Plays a role in neurotransmitter function and has anti-inflammatory properties. Deficiency is linked to cognitive impairment and depression. | Research suggests supplements can improve depressive symptoms, including brain fog. (Healthline) |
| B-Complex Vitamins (B6, B9, B12) | Essential for energy production in brain cells and synthesizing neurotransmitters. B12 deficiency is a known cause of cognitive issues. | Crucial for neurological health, deficiencies can directly cause symptoms of brain fog. (Harvard Health) |
| Magnesium | Important for nerve transmission and has a calming effect on the nervous system. Can improve sleep quality and reduce stress. | Magnesium L-threonate, in particular, has been studied for its ability to cross the blood-brain barrier and enhance cognition. |
| L-Theanine | An amino acid found in green tea that promotes relaxation without drowsiness. When combined with caffeine, it can improve focus and attention. | Studies show it can enhance mental performance and reduce stress. (WebMD) |
Step 3: Master Your Sleep and Reduce Stress
These two pillars are non-negotiable for a clear mind.
- Prioritize Sleep Hygiene: Aim for 7-9 hours of quality sleep per night. Create a routine: go to bed and wake up at the same time, keep your room cool, dark, and quiet, and avoid screens an hour before bed.
- Implement Stress Management: Find what works for you. This could be mindfulness meditation, deep breathing exercises, yoga, spending time in nature, or journaling. Cognitive Behavioral Therapy (CBT) is also highly effective for managing stress and its cognitive impacts.
Step 4: Move Your Body to Clear Your Mind
Regular physical activity is one of the most powerful tools against brain fog.
It boosts blood flow, delivers more oxygen to the brain, and increases levels of Brain-Derived Neurotrophic Factor (BDNF), a protein that supports the growth of new neurons.
Aim for at least 150 minutes of moderate-intensity aerobic exercise (like brisk walking, cycling, or swimming) per week, plus two days of strength training, as recommended by health authorities.
Step 5: Cognitive Training and Brain Exercises
Gently challenge your brain to build cognitive reserve.
This doesn’t have to mean endless Sudoku puzzles.
Engaging in novel and complex activities is key.
Try learning a new language, picking up a musical instrument, or taking a class on a subject that interests you.
These activities forge new neural pathways and can improve mental flexibility.
Brain Fog vs. Dementia vs. Normal Aging
A common fear is that brain fog is an early sign of dementia.
While there can be overlapping symptoms, there are key differences:
- Onset and Progression: Brain fog often has a more sudden or distinct onset, linked to a specific trigger (like an illness, stress, or medication). Dementia, like Alzheimer’s, is typically a slow, progressive decline over years.
- Awareness: People with brain fog are usually acutely aware and frustrated by their cognitive difficulties. In many forms of dementia, insight into one’s own deficits can be lost as the disease progresses.
- Reversibility: Brain fog is often temporary and can be improved or resolved by addressing the underlying cause. Dementia is a neurodegenerative disease that is currently not reversible.
When to See a Doctor About Brain Fog
While lifestyle changes can be very effective, it’s crucial to see a healthcare provider if your brain fog is:
- Persistent or Worsening: It doesn’t improve despite your efforts.
- Impacting Daily Life: It interferes with your ability to work, study, or manage daily responsibilities.
- Sudden and Severe: A rapid change in cognitive function requires immediate medical attention.
- Accompanied by Other Symptoms: Such as severe headaches, numbness, weakness, unexplained weight loss, or fever.
Your primary care physician is a great starting point.
They can run initial tests (like blood work to check for nutrient deficiencies or thyroid issues) and refer you to a specialist like a neurologist, endocrinologist, or rheumatologist if needed.
Frequently Asked Questions (FAQ)
1. How long does brain fog last?
The duration varies widely. If caused by lifestyle factors like poor sleep, it might clear up in days. If linked to a chronic condition like Long COVID or an autoimmune disease, it can last for months or even years, often fluctuating in intensity.
2. Can brain fog be a sign of something serious?
Yes, it can be. While often caused by manageable factors, persistent brain fog can be a symptom of serious underlying conditions like multiple sclerosis, lupus, or significant hormonal disorders. This is why consulting a doctor is essential if it doesn’t resolve.
3. Can supplements cure brain fog?
No supplement is a “cure.” They can help address specific deficiencies (like low Vitamin D or B12) or support overall brain health, but they are most effective as part of a comprehensive approach that includes diet, exercise, sleep, and stress management.
4. Does caffeine help or hurt brain fog?
It’s a double-edged sword. A small amount of caffeine can temporarily boost alertness and focus. However, excessive intake can disrupt sleep, increase anxiety, and lead to a “crash,” ultimately worsening brain fog.
5. Is brain fog a real medical condition?
Brain fog itself is not a formal medical diagnosis. It is a widely recognized term for a set of symptoms of cognitive dysfunction that are very real and can be caused by numerous medical conditions.
6. How is brain fog diagnosed?
A doctor diagnoses the *cause* of brain fog. This involves a detailed medical history, discussion of your symptoms and lifestyle, physical exam, and often blood tests. In some cases, cognitive testing or imaging may be used.
7. Can dehydration cause brain fog?
Absolutely. The brain is about 75% water, and even mild dehydration can impair attention, memory, and other cognitive skills. Staying adequately hydrated is one of the simplest and most effective ways to support mental clarity.
8. What is “fibro fog”?
“Fibro fog” is the specific term used to describe the cognitive dysfunction experienced by people with fibromyalgia. It includes the classic brain fog symptoms of memory loss, difficulty concentrating, and slowed thinking, and is a core feature of the condition.
Conclusion
Brain fog is more than just a fleeting moment of forgetfulness, it’s a significant and often distressing symptom that signals a deeper imbalance in the body.
By understanding its diverse causes—from the stress of modern life to the complex inflammatory pathways of medical conditions—you can begin to take control.
The path to a clearer mind is not about finding a single magic bullet, but about building a resilient foundation through strategic nutrition, restorative sleep, regular movement, and mindful stress reduction.
Start with one small, manageable change today.
Whether it’s adding a serving of leafy greens to your dinner, taking a 15-minute walk, or committing to a consistent bedtime, every step you take is a step toward lifting the fog and reclaiming your focus, energy, and mental sharpness.

